Special Authority (SA)
Special Authority (SA) grants full or partial coverage to a drug or device that otherwise would not be covered or covered only partially. Coverage is provided to patients in specific medical circumstances. This is an overview of Special Authority Coverage — Section 6.3, PharmaCare Policy Manual
SA requests are made by a prescriber. Coverage is approved for patients who meet the published criteria. In exceptional circumstances, SA coverage may be provided when patients don’t meet the criteria or for non-benefit items.
For some drugs, prescribers who have a listed specialty are automatically exempt from submitting an SA request, while for other drugs, listed specialists are invited to enter a Collaborative Prescribing Agreement (CPA) that exempts them from submitting an SA request. In these cases, the drugs get PharmaCare coverage when prescribed by those specialists.
PharmaCare coverage differs from actual reimbursement. Actual reimbursement depends on a patient's PharmaCare plan rules, including Fair PharmaCare deductible and co-payment requirements, and is subject to pricing policies such as the Maximum Pricing Policy, the Low Cost Alternative (LCA) Program and the Reference Drug Program (RDP)
Special Authority requests by pharmacists
Pharmacists may request SA coverage when:
- Prescribing for minor ailments (*contraception does not require SA as it is covered under Plan Z)
- Prescribing OTC medications such as acetaminophen or NRTs for part-fills
- Adapting a prescription
- Applying for exceptional Plan Z coverage
- Dispensing vancomycin following a hospital stay
- Collaborating with prescriber as a BC health authority employee
Pharmacists can also draft a SA request for a prescriber to review, sign and submit.
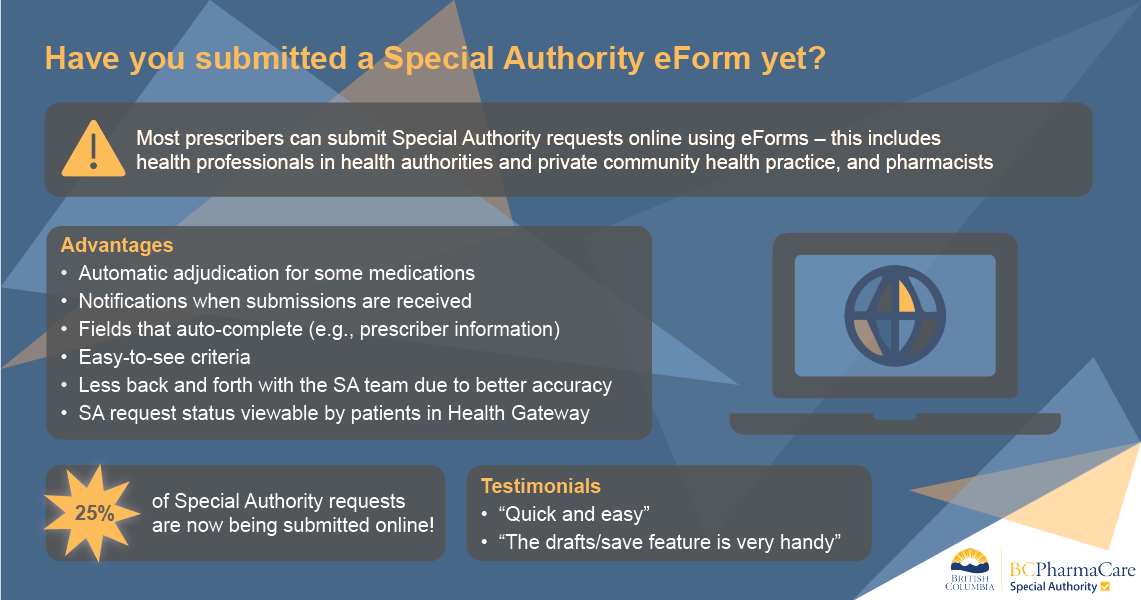
SA requests can be submitted online with eForms or by fax. The online eForms option is easier and quicker than faxing, and generally returns decisions more quickly.
Note: SA approval must be in place before a patient pays for a prescription. Coverage is not retroactive.
SA approval may be granted for the following drug types:
Limited coverage drugs
Medications that generally aren’t first-line therapies or have more cost-effective alternatives. Learn more about limited coverage drugs
Non-reference drugs (partially covered)
Full coverage of non-reference drugs for patients who experience an adverse reaction or treatment failure on the reference drug
Alternative products
If a patient cannot take a fully covered Low Cost Alternative (LCA) drug, prescribers can submit a SA request for full coverage of a brand-name drug in the same LCA category.
Originator biologics and biosimilars
Most originator biologics require SA approval. Those that have biosimilar alternatives are generally covered on an exceptional basis only, for patients who cannot take the biosimilar(s) for documented medical reasons. Refer to Biosimilars Initiative for health professionals
Drugs not marketed in Canada
Health Canada’s Special Access Program drugs are covered in exceptional circumstances only. Refer to Health Canada's Special Access Program Drugs — Section 6.2, PharmaCare Policy Manual
Non-benefit drugs
Non-benefit drugs are considered for coverage on an exceptional, last-resort basis, generally when all available PharmaCare benefit options have been tried without success or are unsuitable for the patient and no other coverage options are available (e.g., third-party insurance). Exceptional approvals are usually for a limited duration.
If faxing, requests must include: a General SA Request form (PDF, 656KB) with Sections 1, 2 and 3 (“requested drug exemption” portion) completed AND a signed letter from the prescriber that includes:
- Patient diagnosis or indication
- A list of all medications tried to date, including dose, duration of trial and patient response to medication, OR, if medications not tried, reasons for not doing so
- The anticipated outcome(s) of treatment with the requested drug (e.g., physical symptoms, quality of life/function)
- Confirmation that the patient has no other insurance that would cover any part of the drug’s cost
- Any additional pertinent information
Getting SA coverage for an LCA or RDP drug
- Go to the SA drug list
- Click on the drug name to view its coverage criteria.
- Check for any practitioner exemptions. If your specialty is in the list, you do not need to submit an SA request. The prescription will be covered automatically.
- Check if a Collaborative Prescribing Agreement (CPA) is available. If you enter into a CPA, you do not need to submit a SA request when prescribing according to the terms of the CPA.
- If you aren't eligible for an exemption or a CPA, follow the instructions for submitting the request in eForms, or download the PDF form linked at the bottom of the drug’s SA criteria page. If faxing, sign the form and fax it to 1-800-609-4884 (toll-free in B.C.).
SA approval must be in place before the patient fills the prescription. Coverage cannot be provided retroactively.
Note: PharmaCare may use PharmaNet records to verify whether criteria have been met. If you provided samples for medication trials, documentation may be required.
For patients who cannot take a fully covered LCA drug
The Low Cost Alternative (LCA) Program ensures B.C. residents get the best value on multiple-source drugs. Each LCA category consists of drugs with the same active ingredient(s) and the same strength. PharmaCare covers only those drugs that meet a set price.
If your patient is allergic to or has an intolerance to non-therapeutic ingredients in the fully covered drugs within an LCA category, you can submit a Special Authority request for full coverage of another drug in that category (including an alternative generic version of the same drug).
- See the LCA Master Spreadsheet that lists the multiple-source drugs that PharmaCare covers. In column F, a P indicates a partial benefit and F indicates a full benefit. Only drugs marked P require SA approval to be covered.
- Complete a general Special Authority request in eForms. If you aren’t enrolled in eForms, complete the fillable PDF version: General Special Authority Request (PDF, 656KB)
Document your patient's clinical need for the drug. Be sure to list all the fully covered products they have tried. - Submit the SA request through eForms. If using a paper form, fax it to 1-800-609-4884 (toll-free in B.C.).
After you submit the request
SA requests are prioritized by date received and by urgency. Once the request is processed, PharmaCare will notify you (the prescriber) of the decision, unless you indicated you do not require confirmation. Patients may also track progress of their SA requests in Health Gateway
Note: Some drugs are eligible for auto-adjudication and will return an immediate decision. Refer to the SA drug list for the ones marked “Yes” in the auto-adjudication column.
Turnaround times
Urgent SA requests are usually processed within one business day. The current turnaround for regular faxed SA requests is 10 weeks. It is strongly recommended that prescribers submit requests through eForms, if applicable, as turnaround times are generally much quicker. Some drugs are eligible for auto-adjudication, which returns immediate decisions. Learn how at SA eForms.
SA requests may be deemed urgent for specific medications (e.g., anticoagulants, oral antifungals, antibiotics, psychiatric and chemotherapy drugs, or drugs for substance use disorder) and circumstances (e.g., hospital discharge, palliative treatment, MAiD, acute mental health conditions or life-threatening conditions). In these cases, all efforts are made to expedite the turnaround time.
SA coverage is valid from the date the approval is entered in a patient's record on PharmaNet. Approval must be in place before a patient fills a prescription, as coverage won’t be provided retroactively. The duration of coverage depends on the drug and the condition being treated.
BC PharmaCare reviews manufacturer drug submissions for PharmaCare coverage. For information on the drug review process, refer to Drug review. If you have questions about the drug review process, contact PharmaCare Formulary Management at drugreviewprocess@gov.bc.ca.
If you have concerns about the criteria used to adjudicate SA drug coverage requests, please send an email to FM.GenericMailbox@gov.bc.ca.
78% of SA requests are approved. General information about appealing a SA decision is on the Special Authority web page. To appeal a SA coverage decision, you will need to fax the original SA request with any pertinent additional supporting information to 1-800-609-4884. PharmaCare does not accept verbal requests for appeals. Appeals are formally reviewed by the Pharmacist Review Committee.
Exceptional funding of EDRDs
On a case-by-case, last-resort basis, PharmaCare covers expensive drugs for rare diseases (EDRDs) that have an estimated annual cost of more than $100,000 per patient. Requests for exceptional, last-resort coverage must be submitted in writing, in a letter containing the following details: baseline objective measurements that determine the patient’s response to treatment, duration of treatment, current dose, rationale for treatment, specific quantitative results considered to be indicators of success, and a list of all therapies that have been previously tried.
- Refer to Exceptional funding for EDRDs

Related links
- SA drug list with links to request forms
- SA request forms by condition
- Limited coverage drugs

Resources for your patients
Subscribe
Enter your email address to subscribe to updates of this page.