Benefits for bargaining unit employees
This 2025 Benefits Guide for Bargaining Unit Employees (PDF, 732KB) provides a comprehensive overview of health and life insurance benefits programs for Bargaining Unit employees. Share the details with your family so you can make the most of your benefits program.
The information provided in this guide is intended to accurately summarize the terms and provisions of the Bargaining Unit Benefits Plan.
In the event of any conflict between the contents of this guide and the actual plans, contracts or regulations, the provisions outlined in those documents apply.
For a quick summary of your benefits, please review 2025 Bargaining Unit Benefits at a Glance (PDF, 167KB).
For a list of forms related to pay and benefits, review the Careers & MyHR forms and tools index.
Employees are responsible for reading the information provided in the Benefit Guide or on Careers & MyHR and contacting AskMyHR (IDIR restricted) if they have any questions.
To enrol for benefits, employees MUST complete the application form(s) before the deadline to be eligible for benefits when coverage begins.
Value of your benefits program
Benefits are an important part of your total compensation package. There's no cost to you to participate in the Extended Health and Dental Plan. The reimbursements you receive under the plan for eligible items and services are paid for by the employer (up to plan limits).
The Employee Basic Group Life Insurance plan provides employee life insurance at a reasonable group premium rate and a portion of your premium is paid by your employer.
On average, your benefits add over 20% to your overall compensation.
Program overview
Your health and life insurance benefits program consist of the following benefit plans that fall into the categories of Core and Optional plans.
Employee Basic Life Insurance is mandatory.
You can waive coverage in any of the remaining plans.
The plans
Core benefits
- Extended health plan
- Dental plan
- Employee Basic Life Insurance (mandatory, but ends when you turn 65)
Optional benefits
- Optional Family Funeral Benefit
- Employee Optional Life Insurance
- Spouse Optional Life Insurance
- Child Optional Life Insurance
- Employee Optional Accidental Death & Dismemberment Insurance
- Spouse Optional Accidental Death & Dismemberment Insurance
- Child Optional Accidental Death & Dismemberment Insurance
Who's eligible for benefits?
Employees
This benefits program applies to:
- Regular bargaining unit employees, including part-time employees
- Auxiliary employees who’ve completed 1,827 hours of work in 33 pay periods with the same ministry
- Auxiliary employees (BCGEU only) who have worked three consecutive years with the same ministry without a loss of seniority and have 1,200 hours of straight time in the past 26 pay periods
- Auxiliary employees who are not eligible for health and welfare benefits receive a compensation allowance as calculated in accordance with the main agreement
You must enrol to be eligible for coverage.
You can extend your benefits to your spouse and to children who meet eligibility requirements. You must enrol your dependents to receive coverage.
Spouse
Your legal or common-law spouse (same or opposite sex) who's living with you is eligible for coverage. By enrolling your common-law spouse in your benefits plans, you're declaring that person as your common-law spouse, and that you've been living in a common-law relationship or cohabiting for at least 12 months. The cohabitation period may be less than 12 months if you claimed your common-law spouse’s child/children for tax purposes. A separate form is not required.
If your spouse is also a BC Public Service employee or is enrolled in a benefits program with an employer outside of the BC Public Service, you can both enrol in your benefits plans, listing the other as a dependent. You may be able to submit your extended health and dental receipts to both plans and receive up to 100% reimbursement (to plan limits) of your eligible expenses.
If you separate from your spouse, they're no longer eligible for coverage under your benefits plan. Any terms and conditions under separation and divorce agreements are the responsibility of the employee, not the employer. Once a common-law spouse has been enrolled in your benefits plan, a different common-law spouse and any eligible dependents may be enrolled in the plan 12 calendar months after you’ve cancelled coverage for the previous common-law spouse and applicable dependents. The waiting period doesn't apply when you're going from legal spouse to a common-law spouse, legal spouse to legal spouse, or common-law spouse to a legal spouse. You're responsible for cancelling your spouse’s coverage when they're no longer eligible for coverage.
Dependent children
Children (natural, adopted, stepchildren or legal wards) are eligible for coverage if they’re unmarried/not in a common-law relationship, mainly supported by you, dependents for income tax purposes and any of the following:
- Under the age of 19
- Under the age of 25 and in full-time attendance at a school, university or vocational institution which provides a recognized diploma, certificate or degree
- Mentally or physically disabled and past the maximum ages stated above. This only applies if they become disabled before reaching the maximum ages, if the disability has been continuous and if the child is covered as a dependent on the employee's benefits when disabled dependent status was approved. The child, upon reaching the maximum age, must still be incapable of self-sustaining employment and must be completely dependent on you for support and maintenance
- Residing with your former spouse who is not eligible for health and dental coverage
A grandchild is not an eligible dependent unless adopted by, or a legal ward of, the employee or the employee’s spouse.
Dependent children over 19
Extended health and dental coverage for a dependent child will automatically end on the date your child turns 19, unless you certify that your child is in full-time attendance at a school, university or vocational institution which provides a recognized diploma, certificate or degree or your child has been approved for coverage as a disabled dependent prior to becoming ineligible for coverage as a dependent child or student.
To certify your child as an eligible student before they turn 19:
- You’ll receive a Confirmation of Dependent Eligibility form from Canada Life
- Submit your Confirmation of Dependent Eligibility form to Canada Life as per instructions on the letter
In subsequent years, return the Confirmation of Student Eligibility form back to the Benefit Service Centre before August 30, advising that your child is a full-time student.
Include your child’s name, date of birth and the school they’re attending. You’re responsible for cancelling coverage for dependent children who are no longer eligible for coverage. Coverage for a dependent child with full-time student status will automatically end at age 25 unless the child has disability status.
To apply for disabled dependent status, you must complete the Application for Over-Age Dependant Coverage form and forward the completed form to Canada Life as per instructions on the form.
Optional life insurance plans do not end automatically; therefore, you must cancel them when your dependents are no longer eligible for coverage under your benefit plan.
|
Benefit |
Regular employee |
Auxiliary employee |
|---|---|---|
|
Extended health and dental plans |
|
|
|
Employee Basic Life Insurance plan |
|
|
|
Optional Family Funeral Benefit |
|
|
| Optional Life and Optional Accidental Death & Dismemberment (AD&D) Insurance |
|
|
Coverage for eligible dependents is effective on the date on which your coverage is effective, or on the first of the month following the date the enrolment form is received by the Benefits Service Centre, whichever is later.
Where evidence of insurability and approval is required, coverage will begin once approval is granted by the carrier. Ensure that the amount on the evidence of insurability form matches the amount of insurance that you have applied for.
Verify that coverage is effective prior to using services.
To check that coverage is in place after you have enrolled, log into My Time and Pay > Employee Self Service > Benefits Summary.
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
For questions regarding coverage submit an AskMyHR (IDIR restricted) service request, using the categories Myself (or) My Team or Organization > Benefits > Bargaining Unit Employees.
How to enrol for the first time
During initial enrolment, you can enrol for extended health and dental coverage immediately, even if you're serving a waiting period.
Extended health and dental coverage will not be effective until your waiting period is over.
For the optional life insurance plans, you must enrol within 31 days of hire as a regular employee, or within 31 days of the day you reach your hours for benefits as an auxiliary employee; otherwise, they will be considered waived.
The optional life insurance plans available are:
- Optional Family Funeral Benefit
- Employee Optional Life Insurance
- Spouse Optional Life Insurance
- Child Optional Life Insurance
- Employee Optional Accidental Death & Dismemberment Insurance
- Spouse Optional Accidental Death & Dismemberment Insurance
- Child Optional Accidental Death & Dismemberment Insurance
After your initial enrolment, you will not be able to make changes to your optional life insurance plans until the annual enrolment period, or until you have an eligible life event.
There's no need to enrol for employee basic life insurance. You're automatically enrolled if you’re under age 65. It's recommended that you complete the Group Life Beneficiary Designation form; otherwise, your life insurance will default to your estate.
Employees can enrol online through My Time and Pay > Employee Self Service > Benefits Summary. By enrolling online, you can to track the status of your application through AskMyHR (IDIR restricted). Complete all forms that are applicable, and you must save them before submitting them.
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
If you don't have access to Employee Self Service, complete the manual forms below that are applicable and send them to the Benefits Service Centre for processing through an AskMyHR (IDIR restricted) service request. Use the categories Myself (or) My Team or Organization > Benefits > Submit a Health Benefit Form/Application.
- Bargaining Unit Benefits Program Enrolment/Change form (PDF, 378KB)
- Group Life Beneficiary Designation (PDF, 174KB)
- Evidence of Insurability (PDF, 518KB) (only required at initial enrolment when applying for Optional Employee and/or Optional Spouse Life Insurance over $50,000)
The original Group Life Beneficiary Designation form must be mailed to the address on the top of the form.
The Evidence of Insurability form should be sent directly to Canada Life. Submission information is on the form.
Choosing life insurance coverage
If you’re under age 65, you're automatically enrolled in Employee Basic Life Insurance as a condition of employment and cannot be waived. You may want to designate a beneficiary (otherwise it defaults to your estate). The rules around when you need to provide evidence of insurability (good health) are outlined below.
Carefully consider the optional life insurance plans available to you during initial enrolment, especially if you (or your spouse) have medical conditions that may prevent you from increasing your life insurance in the future.
The optional life insurance plans available are:
- Optional Family Funeral Benefit
- Employee Optional Life Insurance
- Spouse Optional Life Insurance
- Child Optional Life Insurance
- Employee Optional Accidental Death & Dismemberment Insurance
- Spouse Optional Accidental Death & Dismemberment Insurance
- Child Optional Accidental Death & Dismemberment Insurance
Premiums for these plans can be found under the Benefits at a glance section.
Evidence of insurability (good health)
Not required:
- Up to $50,000 of optional life insurance for yourself and/or your spouse on initial enrolment only
- Child Optional Life Insurance initial enrolment and subsequent increases
- Accidental Death & Dismemberment Insurance initial enrolment and subsequent increases
- Family Funeral Benefit initial enrolment and subsequent enrolment
Required:
- If you choose more than $50,000 of optional life insurance for yourself and/or your spouse during your initial enrolment
- All other increases in life insurance for yourself and/or your spouse
Remember to list your dependents and select them for the benefit on the enrolment form.
To have dependents covered under extended health and dental, you must record their information in the 'Dependent' section of the enrolment form and select the dependents you wish to cover under each benefit plan. Take the time to ensure that your dependent information is correct and that you’ve selected the right dependent(s) for coverage in each plan.
Be sure to designate beneficiaries for your Employee Basic and Optional Life Insurance.
Complete, sign and date a Group Life Beneficiary Designation (PDF, 174KB). If you don’t designate a beneficiary by submitting the signed form, benefits will be paid to your estate in the event of your death. Beneficiary designations are not effective until the completed and signed original form has been received by MyHR.
Submit forms through AskMyHR (IDIR restricted) using the categories Myself (or) My Team or Organization > Benefits > Submit a Health Benefit Form/Application.
Because the Group Life Beneficiary Designation form is a legal document, you must print, sign, date and mail the original document to:
Benefits Service Centre
3980 Quadra Street
Victoria, B.C. V8X 1J9
Once your applications have been processed, you can log into Employee Self Service at any time to view your Benefits Summary (except for your life insurance beneficiaries).
My Time and Pay > Employee Self Service > Benefit Summary
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
Waiting periods may apply and you should verify coverage is in effect prior to purchasing items or services.
PharmaCare registration
All plan members must sign up for PharmaCare. This will assist with prescription coverage, limiting the impact on your lifetime maximum. Do not submit this form to AskMyHR.
How to update your coverage
If you want to add or cancel dependents after your initial enrolment, or make changes to optional life insurance due to an eligible life event or during the annual enrolment period, you'll need to complete and submit the applicable forms.
If you're making changes to your optional life insurance due to an eligible life event or annual enrolment, ensure you complete the application form with your employer as well as the Evidence of Insurability form (if applicable) for Canada Life. The amount of insurance that you're applying for must indicate the total amount of coverage you want on the employer application form (for example: if you currently have $100,000 optional spouse life insurance and you want to increase it to $250,000, you must indicate $250,000 and not only the increased amount of $150,000).
Employees can update their coverage online through My Time and Pay > Employee Self Service > Benefits Summary. By enrolling online, you can track the status of your application through AskMyHR (IDIR restricted).
Complete all forms that are applicable, and you must save them before submitting them.
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
If you don't have access to Employee Self Service, complete the manual forms below that are applicable and send them to the Benefits Service Centre for processing through an AskMyHR (IDIR restricted) service request. Use the categories Myself (or) My Team or Organization > Benefits > Submit a Health Benefit Form/Application.
- Bargaining Unit Benefits Program Enrolment/Change Form (PDF, 378KB)
- Group Life Beneficiary Designation (PDF, 174KB)
- Evidence of Insurability (PDF, 518KB) (only required when applying for or applying to increase Optional Employee and/or Optional Spouse Life Insurance)
The original Group Life Beneficiary Designation form must be mailed to the address on the top of the form.
The Evidence of Insurability form should be sent directly to Canada Life. Submission information is on the form.
Your benefits will be effective on the first of the month following your application.
Changes in coverage take effect as they occur, provided that you're actively at work.
Waiting periods may apply and you should verify that coverage is in effect prior to purchasing items or services.
There are two opportunities where you can update your optional life insurance plans after your initial enrolment (evidence of insurability may be required).
- Once a year during the annual enrolment period, for the change to be effective April 1 of that year, applications must be received by the end of the enrolment period in February.
The optional life insurance plans available are:- Optional Family Funeral Benefit
- Employee Optional Life Insurance
- Spouse Optional Life Insurance
- Child Optional Life Insurance
- Employee Optional Accidental Death & Dismemberment Insurance
- Spouse Optional Accidental Death & Dismemberment Insurance
- Child Optional Accidental Death & Dismemberment Insurance
- During an eligible life event which allows you to make changes to your optional life insurance plans within 60 days of the event.
Life events include:- Marriage or entering a common-law relationship
- Divorce, separation or the end of a common-law relationship
- Birth or adoption of a child
- Loss of a child’s status as a dependent (marriage, age limit, no longer a student)
- Change in your child’s eligibility that allows coverage under the program
- Your spouse gains or loses benefits
- Death of a spouse or child
Baby enrolment/addition of a newborn
The easiest way to enrol your newborn for the Medical Services Plan (MSP) is to complete the Online Birth Registration through the Vital Statistics Agency. They will send your baby’s information to Health Insurance BC (HIBC).
Effective dates of coverage
Changes will be effective on the appropriate date based on annual enrolment, an eligible life event, or the approval of evidence of good health for life insurance.
- Changes made during annual enrolment will be effective April 1
- Changes made as a result of an eligible life event will be effective on either the date of the event or the form signature date, whichever is later, provided either date occurs within 60 days of the life event. If a life event is reported more than 60 days after the event, changes to your options will not be permitted at that time
- Exceptions, back dating and retroactive adjustments will not be made
- Review your coverage and make changes during the enrolment period or as soon as possible after the eligible life event to ensure that MyHR receives your benefits change forms no later than 60 days from the date of the event
| Extended health plan | Coverage |
|---|---|
| Annual deductible |
$100 |
| Reimbursement |
Reimbursed at 80% for the first $2,000 paid in a calendar year per person and then 100% for the balance of the year (subject to some restrictions and plan maximums) |
| Lifetime maximum |
$3 million (includes coverage for out-of-province or out-of-country medical emergencies) |
| Prescription drugs |
Covered drugs and medicines purchased from a licensed pharmacy, which are dispensed by a pharmacist, physician or dentist subject to PharmaCare’s policies including reference based pricing and lowest cost alternative |
| Vision |
$250/24 months for adults |
| Paramedical services (chiropractor, massage therapy, naturopathic physician, physiotherapy, podiatry) |
Acupuncture, chiropractor, naturopathic physician and podiatry: $500/year/person |
| Dental plan | Reimbursement | Coverage |
|---|---|---|
| Basic services | 100% |
Cleaning, polishing, topical fluoride: once every nine months for adults, once every six months for dependent children |
| Major services | 65% |
Services required for reconstruction of teeth and for the replacement of missing teeth (for example: crowns, bridges and dentures) |
| Orthodontic services | 55% |
Coverage for orthodontic services provided to maintain, restore or establish a functional alignment of the upper and lower teeth Lifetime maximum is $3,500/covered person |
| Employee Basic Life Insurance (to age 65) |
Premium |
Coverage |
|---|---|---|
| Mandatory coverage | Premium for the first $100,000 of insurance coverage is employer-paid. Employee-paid monthly premium for coverage above $100,000 is 9 cents per thousand dollars | Coverage is equal to three times annual salary or employer-paid minimum coverage ($100,000), whichever is greater. Includes accidental dismemberment insurance, loss of sight insurance, and terminally ill advance payment |
| Optional Family Funeral Benefit | Premium | Coverage |
|---|---|---|
| Optional coverage |
$2.16/month ($25.92/year) |
Life insurance in the amount of $10,000 for spouse and $5,000 per dependent child |
|
Optional Accidental Death & Dismemberment Insurance |
Units of |
Maximum |
Annual rate per unit |
|
You |
$25,000 |
$500,000 |
$9.60 |
|
Your spouse |
$25,000 |
$500,000 |
$9.60 |
|
For all your dependent children |
$10,000 |
$250,000 |
$3.30 |
| Optional Life Insurance | Units of | Maximum |
|---|---|---|
| You | $25,000 | $1 million |
| Your spouse | $25,000 | $500,000 |
| For all your dependent children | $5,000 | $20,000 (cost for all dependent children is $11.28 per unit of $,5000) |
| Gender/age (yrs)* | Under 35 | 35 to 39 | 40 to 44 | 45 to 49 | 50 to 54 | 55 to 59 | 60 to 64 |
|---|---|---|---|---|---|---|---|
| Female (NS) | $9 | $12 | $18 | $30 | $48 | $84 | $108 |
| Female (S) | $12 | $18 | $30 | $60 | $90 | $138 | $192 |
| Male (NS) | $18 | $18 | $24 | $48 | $87 | $144 | $189 |
| Male (S) | $30 | $36 | $60 | $102 | $177 | $294 | $396 |
*Premiums are not locked in at the rate in place when application is made and will change as the age of the enrolled individual changes.
During initial enrolment, employees have 31 days to apply for up to $50,000 of Employee Optional and/or Spouse Optional Life Insurance evidence free.
Evidence of insurability is required for any amounts over $50,000 during initial enrolment and for all future increases. Applications must be approved before coverage can begin.
Tips
- To submit eClaims, register and log into My Canada Life at Work, Canada Life's plan member website. My Canada Life at Work provides online access to your personalized extended health and dental coverage and claims information
- Claiming deadline for extended health and dental is 15 months from the date the expense was incurred
- Ask your doctor or pharmacist if there's a less expensive generic medication that is right for you
- Don’t forget to update your benefits coverage as your personal circumstances change
- Remember to designate a beneficiary for your group life insurance
- Naming a beneficiary for your Public Service Pension Plan is a separate process from nominating your group life insurance beneficiary. For more information, contact the Public Service Pension Plan
Medical Services Plan
Impact to extended health plan
New or returning to B.C.
- First visit an ICBC office to obtain a BC Services card and
- Then apply for MSP coverage
Leaving B.C.
Leaving British Columbia temporarily can impact your continued coverage under MSP. More information related to both temporary and permanent absences from B.C. is available in the Leaving B.C. brochure.
To request MSP account changes (for example: address changes, adding or removing dependents, or re-certifying your child as a full-time student) and/or to submit documentation online, please visit the Managing Your MSP Account page.
Questions
The extended health plan is designed to partially reimburse you for a specific group of medical expenses which are not covered by the Medical Services Plan or the PharmaCare program.
Overview
Canada Life administers your extended health plan on behalf of your employer. Detailed descriptions of expenses eligible for reimbursement under this plan are provided in the table below.
There's a lifetime maximum of $3 million per covered person, which includes coverage for out-of-province or out-of-country medical emergencies. This lifetime maximum may be reinstated after paying for any one serious illness based on satisfactory evidence provided by the employee to the carrier of complete recovery and return to good health.
This is an employer-paid, non-taxable benefit.
Reimbursement
Before you receive reimbursements, you must fulfil the $100 annual deductible unless you're claiming for reimbursement of an expense not subject to the annual deductible.
Unless otherwise stated, you'll be reimbursed at 80% of the first $2,000 paid in a calendar year per person, and then 100% for the balance of the year (subject to some restrictions and plan maximums).
It's your responsibility to verify that an item or service is covered prior to purchase. A claim for a service or supply that was purchased from a provider that is not approved by Canada Life may be declined. Contact Canada Life if the item is not listed in this guide. It's recommended that you get an expense pre-approved if the cost is over $1,000.
What's covered by your extended health plan
The following is a list of expenses eligible for reimbursement under the extended health plan when incurred as a result of a necessary treatment of an illness or injury and, where applicable, when ordered by a physician and/or surgeon. Check My Canada Life at Work for detailed information or contact Canada Life at 1-855-644-0538.
| Feature | Coverage |
|---|---|
| Accidental injury to teeth |
Dental treatment by a dentist or denturist for the repair or replacement of natural teeth or prosthetics, which is required and performed and completed within 52 weeks after an accidental injury that occurred while covered under this plan. No reimbursement will be made for temporary, duplicate or incomplete procedures, or for correcting unsuccessful procedures. Expenses are limited to the applicable fee guide or schedule. Accidental means the injury was caused by a direct external blow to the mouth or face resulting in immediate damage to the natural teeth or prosthetics and not by an object intentionally or unintentionally being placed in the mouth. |
| Acupuncture |
Acupuncture treatments performed by a medical doctor or an acupuncturist registered with the College of Traditional Chinese Practitioners and Acupuncturists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $500/year/person. |
| Braces, prosthetics and supports |
To be eligible for reimbursement, you must include a practitioner’s note for all prosthetics, braces and supports to confirm the medical need for the device. Accepted practitioners include licensed chiropractors, physiotherapists and physicians. The prescription must include the medical condition and the braces must contain rigid material. |
| Breast prosthetics |
See the 'Mastectomy forms and bras' section of this table for more information. |
| Chiropractor |
Chiropractic treatments performed by a chiropractor registered with the College of Chiropractors of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $500/year/person. X-rays taken by a chiropractor are not eligible for reimbursement. |
| Contraceptives |
Please contact Canada Life or log into My Canada Life at Work for Plan Members and enter the product DIN to confirm if the prescribed contraceptive is covered.
|
| Counselling (registered clinical counsellor, registered clinical psychologist, recognized social worker) |
Service fees of a recognized social worker, registered clinical psychologist or counsellor—payable to a maximum of $750/year/covered individual. The practitioner must be registered in the province where the service is rendered. To determine if a psychologist is registered for claiming purposes, contact the College of Health and Care Professionals of BC at 604-742-6715 (toll-free 1-877-742-6715) or use the searchable registry at https://chcpbc.org/. To determine if a counsellor is registered for claiming purposes, contact the BC Association of Clinical Counsellors at 250-595-4448 (toll-free 1-800-909-6303) or use the searchable registry at https://bcacc.ca/counsellors/. To determine if a social worker is qualified for claiming purposes, contact the BC College of Social Workers at 604-737-4916 (toll-free 1-877-576-6740) or use the searchable registry at https://bccsw.ca.thentiacloud.net/webs/bccsw/register/#/. Visit Careers & MyHR for information about short-term counselling available through the Health and Well-being program. |
| Drugs and medicines |
Covered drugs and medicines purchased from a licensed pharmacy, which are dispensed by a pharmacist, physician or dentist subject to PharmaCare’s policies including reference-based pricing and lowest cost alternative. Drugs and medicines include:
Reimbursement of eligible drugs and medicines will be based on a maximum dispensing fee of $7.60 and a maximum mark-up of 7% over the manufacturer’s list price. All plan members must sign up for PharmaCare to assist with prescription coverage, limiting the impact on your lifetime maximum. Unless medical evidence is provided to Canada Life that indicates why a drug is not to be substituted, Canada Life can limit the covered expense to the cost of the lowest priced interchangeable drug. Prior authorization: Canada Life requires prior authorization to provide appropriate drug treatment and to ensure the drugs prescribed are considered reasonable treatment for the condition. For brand name drugs, your physician will have to complete a Request for Brand Name form to provide medical evidence that the generic version has adverse side effects. For more information regarding prior authorization and specialty drug processes, sign in to My Canada Life at Work and click on Info centre > Benefits information sheet, or see the 'Prior authorization and specialty drugs' section. No benefits will be paid for:
|
| Emergency ambulance services |
Emergency transportation by licensed ambulance to the nearest Canadian hospital equipped to provide medical treatment essential to the patient. Air transport when time is critical, and the patient’s physical condition prevents the use of another means of transport. Doctor’s note may be required. Emergency transport from one hospital to another only when the original hospital has inadequate facilities. Charges for an attendant when medically necessary. |
| Examinations: medical |
Medical examinations rendered by a physician, required by a statute or regulation of the provincial and/or federal government for employment purposes, for you and all your registered dependents provided such charges are not otherwise covered. |
| Examinations: vision |
Fees for routine eye examinations to a maximum of $100/24 months/person for adults who are age 19 or older, when performed by a physician or optometrist. Exams for persons under age 19 and over age 64 are covered under the Medical Services Plan. The balance not covered by the Medical Services Plan for individuals over age 64 is eligible for reimbursement under this extended health plan to plan maximum. |
|
Hairpieces and wigs |
Hairpieces and wigs, when medically necessary, are eligible for reimbursement to a maximum of $500/24 months. |
| Hearing aids and repairs |
When prescribed by a physician or audiologist, reimbursements at $1,500/ear/48 months for adults and $1,500/ear/24 months for children. This benefit is not subject to an annual deductible. The prescription must be included with the claim. Batteries, recharging devices or other such accessories are not covered. |
| Hospital charges |
Additional charges for semi-private or private accommodation over and above the amount paid by provincial health care for a normal daily public ward while you're confined in a hospital under active treatment. This doesn't include telephone or TV rental or other amenities. |
| Massage therapy |
Massage treatments performed by a massage practitioner registered with the College of Massage Therapists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $750/year/person. X-rays taken, and drugs, medicines or supplies recommended and prescribed by a massage therapist are not covered. |
| Mastectomy forms and bras |
Mastectomy forms and bras are eligible for reimbursement to a maximum of $1,000/12 months. |
| Medical aids and supplies |
A variety of medical aids and supplies as follows: For diabetes:
NOTE: To be eligible for CGM coverage, you must first apply for coverage through BC PharmaCare Special Authority. Portions of the cost that are not paid by BC PharmaCare, such as the deductible and the coinsurance amount, can be claimed under the extended health plan.
NOTE: If you switch from using testing supplies to an insulin injector, testing supplies are not covered for the next 60 consecutive month period.
Standard durable equipment as follows: The cost of renting, where more economical, or the purchase cost of durable equipment for therapeutic treatment including:
Pre-authorization is recommended for items costing over $1,000 and is required for items over $5,000. |
| Naturopathic physician |
Naturopathic services performed by a naturopathic physician licensed by College of Naturopathic Physicians of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $500/year/person. X-rays taken, and drugs, medicines or supplies recommended and prescribed by a naturopathic physician are not covered. |
| Needleless injectors |
When prescribed by a physician:
|
| Orthotics and orthopedic shoes |
When prescribed by a physician or podiatrist when medically necessary, custom-fit orthotics or orthopedic shoes, including repairs, orthotic devices and modifications to stock item footwear but not including arch supports/inserts. Payable to a maximum of $400/person/calendar year. Not all casting techniques are approved for coverage, so please confirm with Canada Life prior to purchase. Custom-made orthotics When submitting claims for custom-made orthotics, include the following information:
Custom-made orthopedic shoes When submitting claims for custom-made orthopedic shoes, include the following information:
|
| Out-of-province/out-of-country emergencies |
Reasonable charges for a physician’s services due to an emergency are eligible for reimbursement, less any amount paid or payable by the Medical Services Plan, subject to the lifetime maximum of $3 million for extended health and out-of-province/out-of-country travel. |
|
Paramedical services (acupuncture, chiropractor, massage therapy, naturopathic physician, physiotherapy, podiatry) |
Services provided by licensed paramedical practitioners. For the purposes of this plan, paramedical services are a defined group of services and professions that supplement and support medical work, but don't require a fully qualified physician. These services include:
Acupuncture, chiropractor, naturopathic physician and podiatry: $500/year/person Massage therapy: $750/year/person Physiotherapy: $2,000/year/person Claims will be reimbursed at 80% of the cost from the first visit, subject to reasonable and customary limits (R&C) until the annual maximum is reached. R&C represents the standard fees healthcare practitioners would charge for a given service. They're reviewed regularly and are subject to change at any time. If your healthcare practitioner charges more than a R&C limit, you'll be responsible for paying the difference. For R&C charges, log into My Canada Life at Work, go to Coverage & Balances, Health (50088) and Customary charges to view. If you have any questions about R&C limits for a given service, contact Canada Life at 1- 855-644-0538. |
| Physiotherapist |
Professional services performed by a physiotherapist registered with the College of Physical Therapists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $2,000/year/person. |
| Podiatrist |
Professional services performed by a podiatrist registered with the British Columbia Association of Podiatrists. See the 'Paramedical services' section of this table for information about reasonable and customary limits. Coverage is $500/year/person. X-rays taken, or other special fees charged by a podiatrist are not covered. |
| Prostate-serum antigen test |
Once per calendar year. |
| Smoking cessation products |
Drugs and supplies for prescriptions and non-prescription smoking cessation. Maximum: $300/year/person to a lifetime maximum of $1,000. You must register with the Quittin’ Time Program prior to purchasing any products.
|
| Vision care |
This benefit is not subject to the annual deductible and is reimbursed at 100% (to benefit plan limits). Purchase and/or repair of corrective eyewear, charges for contact lens fittings and laser eye surgery, when prescribed or performed by an optometrist, ophthalmologist, or physician. Corrective eyewear includes lenses, frames, contact lenses, prescription sunglasses, prescription safety goggles and vision care repairs. Charges for non-prescription eyewear are not covered. A combined maximum of:
Check My Canada Life at Work to verify your personal eligibility period as coverage for vision care is determined using a rolling eligibility date. Eye exams are a separate feature. See the 'Examinations: vision' section of this table for information about eye exams. No benefits will be paid for vision care services and supplies required by an employer as a condition of employment. |
Any item not specifically listed as being covered under this plan is not an eligible item under this extended health plan.
Extended health general exclusions
No benefits will be paid for:
- Expenses that private benefit plans are not permitted to cover by law
- Services or supplies for which a charge is made only because the person has coverage under a private benefit plan
- The portion of the expense for service or supplies that is payable by the government health plan in the person’s home province, whether or not the person is actually covered under the government health plan
- Any portion of services or supplies which the person is entitled to receive or for which they are entitled to a benefit or reimbursement by law or under a plan that is legislated, funded or administered in whole or in part by a government plan without regard to whether coverage would have otherwise been available under this plan
- Services or supplies that do not represent reasonable treatment
- Services or supplies associated with treatment performed for cosmetic purposes only
- Services or supplies associated with recreation or sports rather than with other regular daily living activities
- Services or supplies associated with the diagnosis or treatment of infertility or contraception except as may be provided under the prescription drug provision
- Services or supplies associated with a covered service or supply unless specifically listed as a covered service or supply, or determined by the plan administrator to be a covered service or supply
- Extra medical supplies that function as spares or alternatives
- Services or supplies received outside Canada except as provided under the out-of-country care provision
- Services or supplies received out-of-province in Canada, unless:
- the person is covered by the government health plan in their home province, or the government coverage replacement plan sponsored by the employer, and
- this plan would have paid benefits for the same services or supplies if they have been received in the person’s home province
- Medical evacuation services covered under the employer’s global medical assistance plan
- Expenses arising from war, insurrection or voluntary participation in a riot
- Hospital care for conditions where significant improvement or deterioration is unlikely within the next 12 months. This is considered chronic care
Out-of-province/out-of-country emergency coverage under the extended health group plan
If you're covered under the Provincial Government Medical Service Plan and the extended health group plan (meaning you haven’t waived coverage) and you travel out-of-province or out-of-country for business or personal travel, you're covered for medical emergencies—including those resulting from pre-existing conditions (except for a few exclusions) up to the combined extended health lifetime maximum of $3 million per person.
Your spouse and/or dependents covered under the Provincial Government Medical Service Plan and your extended health group plan are also covered for medical emergency travel benefits while travelling for pleasure. Eligible emergency medical expenses are subject to the annual deductible and will be reimbursed at 100% (to plan maximums).
Eligible emergency out-of-province/out-of-country expenses
- Local ambulance services when immediate transportation is required to the nearest hospital equipped to provide the treatment essential to the patient
- The hospital room charge and charges for services and supplies when confined as a patient or treated in a hospital. Members should contact Travel Assistance for assistance if they have a medical emergency. Refer to the Travel Assistance Brochure (PDF, 2MB) for contact information. When the patient’s medical condition permits, they'll be returned to Canada. Canada Life's standard out-of-country confinement is up to a semi-private ward rate
- Physician, laboratory and x-ray services
- Prescription drugs
- Other emergency services and/or supplies, if Canada Life would've covered the expenses in your province/territory of residence
- Medical supplies provided during a covered hospital confinement
- Paramedical services provided during a covered hospital confinement
- Medical supplies provided out of hospital if you would've been covered in Canada
- Out of hospital services of a professional nurse
These expenses are eligible in a medical emergency only, and when ordered by the attending physician. A medical emergency is:
- A sudden and unexpected injury
- The onset of a condition not previously known or identified prior to departure from B.C. or Canada
- An unexpected episode of a condition known or identified prior to departure from B.C. or Canada
An unexpected episode means it would not have been reasonable to expect the episode to occur while travelling outside of Canada. If a person was suffering from symptoms before departure from Canada, Canada Life may request medical documentation to determine whether, in the circumstances, it could have reasonably been anticipated that the person may require treatment while outside Canada.
Non-emergency continuing care, testing, treatment, surgery and amounts covered by any government plan and/or any other provider of health coverage are not eligible.
Exclusions
- Expenses incurred due to elective treatment and/or diagnostic procedures
- Complications related to such treatment expenses incurred due to therapeutic abortion, childbirth, or complications of pregnancy occurring at week 35 or later, or if high risk, during pregnancy
- Charges for continuous or routine medical care normally covered by the government plan in your province/territory of residence
Business travel medical insurance
Employees without extended health coverage through their employment with the BC Public Service are not covered under the group business travel insurance plan. There are limited exceptions. Employees without extended health coverage should confirm their travel medical insurance status before making travel arrangements. If out-of-province or out-of-country business travel is required, employees without coverage under the corporate travel medical policy should purchase an individual travel insurance plan and claim the expense through their travel claim. When purchasing travel insurance, make sure to read and understand the fine print. Most individual travel insurance plans exclude coverage for pre-existing conditions. Employees should carefully consider their personal health circumstances before agreeing to travel for work.
Optional medical travel insurance
Canada Life has a travel insurance website to enable you to purchase optional travel medical insurance. For more information, review Canada Life’s Optional Emergency Travel Medical Benefit Information Sheet (PDF, 141KB). This travel medical insurance is first payer to your group plan with Canada Life, and you’ll save 10% by purchasing it from this website.
If you have other similar coverage, such as through a credit card plan or another group or individual insurance plan, claims will be coordinated within the guidelines for out-of-province/out-of-country coverage issued by the Canadian Life and Health Insurance Association.
To apply, you'll need your Canada Life group plan number (50088) and your identification number from your Canada Life ID card.
This travel insurance has a maximum amount payable per covered trip of $2 million Canadian. Single or annual travel policies are available if you're under age 80. There are exclusions for pre-existing conditions.
Travel Assistance
Canada Life's Travel Assistance provides assistance if you or an eligible dependant experience a medical emergency while traveling out-of-province/out-of-country. Trained personnel who speak various languages will provide advice and coordinate services for you. This service is available 24 hours a day, 365 days a year and assists members in locating hospitals, clinics and physicians.
Travel Assistance also provides the following services:
- Medical advisers
- Advance payment when required for hospital admission
- Helping to locate qualified legal assistance, local interpreters and appropriate services for replacing lost passports
- Assisting unattended children
- Return of vehicle
- Transportation reimbursement
- Medical evacuation
- Travelling companion expenses
- Transportation of remains if a plan member dies while travelling, expenses for preparing and transporting the plan member’s remains home are covered. The assistance company can also help make the appropriate arrangements
Travel Assistance provides advice and coordinates services at no additional charge. However, it's not a means of paying for any healthcare expenses that you may require. The actual cost for any service(s) received is your responsibility. Some of these expenses may be claimed through:
- Medical Services Plan of BC
- Travel insurance purchased by you
- Your extended health plan
Please ensure that you have the Travel Assistance phone numbers with you when you travel.
Canada Life has simplified the phone numbers and you will just require the following numbers:
- Canada or U.S. 1-855-222-4051
- All other locations 1-204-946-2577
You can find these phone numbers, as well as your plan and personal ID numbers, on your digital benefits ID card available through My Canada Life at Work. Be sure to have access to those numbers and your provincial health care number when you travel for personal identification.
See the Travel Assistance page for more information.
Out-of-country non-emergency coverage
The following non-emergency services and supplies are covered when out-of-country, if benefits would have been paid for the same services and supplies had they been incurred in Canada, subject to the same deductibles, maximums, reimbursements and limitations of the plan.
- Ambulance services
- Prescription drugs
- Medical supplies
- Paramedical services
- Vision care
- Dental accident treatment
Canada Life’s prior authorization process is designed to provide an effective approach to managing claims for specific prescription drugs.
How prior authorization works
Prior authorization requires that you request approval from Canada Life for coverage of certain prescription drugs. When a claim is submitted for any of these drugs, they'll ask for information to help them assess the claim. Your request must be approved before your claim is paid. To ensure your claim is processed without delay, please provide all necessary information before filling a prescription.
Why we require prior authorization
Drugs that are approved for one or more medical conditions are sometimes prescribed for other conditions without being proven as an effective treatment. The practice of requesting additional information is designed to help:
- Provide coverage for appropriate drug treatment
- Ensure the drugs prescribed are considered reasonable treatment for the condition
- Keep your drug plan affordable and accessible
Drugs requiring prior authorization
Canada Life maintains a limited prior authorization drug list with corresponding forms.
Before a claim for any of these drugs is approved, they review the circumstances to determine whether the drug is a reasonable treatment for the condition it was prescribed for.
The prior authorization drug forms list does change. Your group benefits plan may not provide coverage for all of the prior authorization drugs listed, as coverage depends on the terms of your plan.
To view the prior authorization drug forms list, sign in to My Canada Life at Work > Info Centre > Forms > Prior authorizations (tab) to determine which drugs requires prior authorization.
If you have questions about what drugs are covered by your plan, call Canada Life's Group Customer Contact Services office at 1-855-644-0538.
How to request prior authorization
If you’re prescribed a drug that requires prior authorization, you must complete the appropriate section(s) of the drug-specific prior authorization form with your prescribing doctor and submit the form to Canada Life.
Your claim cannot be considered for reimbursement until they receive this form.
If you anticipate submitting a claim for a drug that requires prior authorization, take the appropriate prior authorization form to your doctor’s appointment.
Completed forms can be emailed, faxed or mailed to Canada Life.
Email
cldrug.services@canadalife.com
Fax
Canada Life
Fax Number: 1-204-946-7664
Attention: Drug Claims Management
Mail
Canada Life
Attention: Drug Claims Management
P.O. Box 6000
Winnipeg MB R3C 3A5
If your claim is approved, in most cases, additional prior authorization forms for the drug will not be required. Future claims for the drug will be processed in the same manner as prescription drugs that don't require prior authorization.
Certain drugs may require additional approval after a specified period. In these situations, you may be asked to provide further information regarding the progress of your treatment.
All requests for prior authorization are reviewed by Canada Life. Their decision is based on the information provided to determine whether the prescribed drug represents reasonable treatment.
Notification regarding the claim decision
Once Canada Life reviews your completed prior authorization form, they'll advise you by letter if the request for prior authorization has been approved or not. If the request is declined, you may wish to discuss your medication needs with your doctor or pharmacist. You have the option of paying for the total cost of the drug yourself.
Specialty drug program
Canada Life’s enhanced drug coordination process coordinates eligible drugs under specific provincial programs. You may be required to apply to the provincial program for drug coverage. Some drugs included in this program are also under prior authorization.
How the specialty drug program works
You go to your pharmacy to fill a prescription.
1. The drug is included in the specialty drug program.
- The claim will be paid, but you’ll need to apply to your provincial program
- You’ll receive a letter to apply to the provincial program and respond to Canada Life within 70 days
- Canada Life will coordinate your drug plan with your provincial plan
OR
2. The drug is included in specialty drug program and the prior authorization program.
- If your claim is denied, you’ll receive a letter to apply to your provincial program
- If approved, Canada Life will pay any amounts not eligible under the provincial program
- If the provincial plan declines your claim, send the prior authorization form to Canada Life to assess eligibility under the drug program
- You’ll be notified if your claim is accepted or not
Prescription drug coverage: BC Public Service extended health plan
The following information provides details of the prescription drug coverage under the extended health plan for BC Public Service employees.
What's BC PharmaCare and how does it coordinate with your drug plan?
BC PharmaCare helps all B.C. residents with the cost of eligible prescription drugs, even if you have private drug coverage through the BC Public Service extended health plan. If you fill a prescription that's eligible with BC PharmaCare, BC PharmaCare will start paying for these drugs once your total annual prescription costs reach your deductible—which is based on 3% of your net family income. Your extended health plan will pay your deductible portion in accordance to the plan’s reimbursement limits until the deductible is satisfied, and then PharmaCare will start paying for you and your dependants’ eligible drugs for the rest of the calendar year.
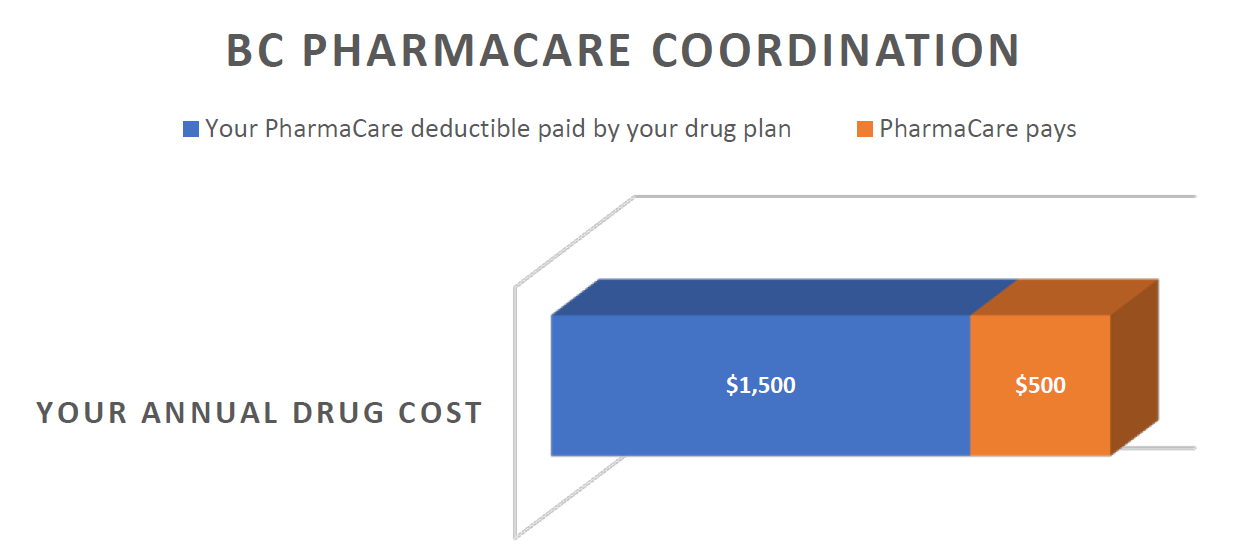
In the example pictured below, based on a net family income of $50,000 and total eligible family drug costs of $2,000 for the year, BC PharmaCare will start paying after your family’s eligible drug costs have reached $1,500 ($50,000 x 3%) within a calendar year.
How does PharmaCare know how to calculate my deductible?
You must register for Fair PharmaCare for BC PharmaCare to access your income tax returns to calculate your deductible. If you don't register, your deductible will be set at the maximum of $10,000, which will add unnecessary costs to your drug plan.
What if I haven't registered with Fair PharmaCare?
If the eligible drug costs for you and your dependant(s) have accumulated and reached a certain threshold within a calendar year, then Canada Life will notify you that you need to register for Fair PharmaCare or your drug claims will be temporarily suspended until Canada Life receives confirmation of Fair PharmaCare registration. Learn more about Fair PharmaCare.
In addition to coordinating drug costs with BC PharmaCare, the drug plan for BC Public Service employees follows BC PharmaCare’s pricing policies which includes the Low Cost Alternative (LCA) Program and the Reference Drug Program (RDP).
What's the Low Cost Alternative (LCA) program?
When the same drug is made and sold by more than one manufacturer, the plan covers the less costly version. Drugs deemed the 'lowest cost alternative' are usually (but not always) generics. The LCA drugs (usually generics) are fully covered by the plan but the more costly brand name drugs are only partially covered up to the LCA price.
For example:
- Celexa™ is the brand version of a popular antidepressant
- The cost of one Celexa 20mg tablet = $1.52 (partially covered)
- The generic version of one Celexa 20mg = $0.26 (fully covered)
Your drug plan would only pay up to the cost of the generic version ($0.26) if you filled a prescription for Celexa™, subject to the terms of your group benefits plan. To get fully reimbursed, you would need to purchase the generic version which can easily be done by the pharmacist without authorization from your doctor.
If there's a medical reason which requires you to take the brand name drug, ask your physician to complete a Request for Brand Name Drug Coverage form (available on the Canada Life website) to provide the medical information on why you require the brand name drug.
What's the Reference Drug Program (RDP)?
Sometimes there are several drugs that treat the same illness or condition that are very similar in effectiveness, chemical structure, and safety.
There are seven therapeutic classes in the Reference Drug Program.
- Angiotensin receptor blockers for high blood pressure
- Proton pump inhibitors for acid reflux and ulcers
- Statins for high cholesterol
- H2 blockers for acid reflux
- Calcium channel blockers for high blood pressure
- Angiotensin converting enzyme inhibitors for high blood pressure
- Non-steroidal anti-inflammatories for pain and inflammation
PharmaCare reviews the cost of the drugs within each category and determines the maximum daily cost it will cover.
Each therapeutic category has reference drugs which are the most cost effective and these are fully covered by the plan, in accordance to the plan’s reimbursement formula. However, the more expensive drugs within a therapeutic category are considered non-reference drugs and these will only be partially covered, up to the maximum daily price.
For example, let’s consider the statins, a popular class of drugs for high cholesterol:
- Reference statin drugs: atorvastatin and rosuvastatin are fully covered
- Non-reference statin drugs: fluvastatin, lovastatin, pravastatin, simvastatin are only reimbursed to a daily maximum of $0.26
Can I get fully reimbursed for a non-reference drug within the Reference Drug Program if my doctor thinks it's medically necessary?
If your doctor thinks it's medically necessary for you to take a non-reference drug because you have already tried a reference drug and it hasn't been effective, you may ask your doctor to apply to BC PharmaCare’s Special Authority Program on your behalf.
Once approved, you can send in the form to Canada Life to get a pricing exception and full coverage, to plan limits, for your non-reference RDP drug.
For any additional information regarding the Reference Drug Program, please refer to the PharmaCare website.
What if I'm already at the pharmacy and realize that my doctor prescribed a non-reference drug? What can I do to get the drug changed to a fully covered drug?
You can go back to your doctor and ask them to prescribe a reference drug within that therapeutic category or ask your pharmacist if they have the ability to adapt the prescription to a reference drug.
Under very limited conditions, pharmacists in British Columbia can change certain prescriptions from one drug to another without consulting your doctor.
BC PharmaCare’s Special Authority drugs
In addition, some drugs may be eligible for coordination with BC PharmaCare’s Special Authority (SA) program. If you're claiming a drug included in the (SA) program, you may be eligible for coverage under the government plan.
Your pharmacy will submit your claim to the provincial program and if approved, the decision will be automatically shared with Canada Life.
If you are declined by the provincial program, a copy of the BCSA application form with the provincial decline included on the form can be sent to Canada Life at:
Canada Life Drug Claims Management
Email
cldrug.services@canadalife.com
Mail
P.O. Box 6000
Winnipeg MB R3C 3A5
Fax
1-204-946-7664
Dental plan
The dental plan is designed to assist you with the cost of your dental care and reimburses most basic and major dental and orthodontic services.
Overview
Canada Life administers your dental plan on behalf of your employer. Dental coverage is available for services in B.C. and for emergency dental services while traveling anywhere outside of B.C. The plan will cover eligible expenses up to the amount it would have covered had the services been performed in B.C.
What's covered by your dental plan?
Dental services fall into three categories:
- Basic preventative and restorative services
- Major services
- Orthodontic services
Reimbursement
Dentists set their own rates for service, but reimbursement of dental fees under this group plan is subject to the dental fee schedule published by the BC Dental Association for dentists, dental specialists, and denturists to plan limits.
You're responsible for any fees that exceed plan limits. Always ask for pre-approval.
You'll be reimbursed 100% to plan limits for the cost of the basic dental services outlined below. If services are performed by a specialist, the fee is equal to that of the general practitioner, plus 10%.
It's your responsibility to verify that an item or service is covered prior to treatment. A claim for a service or supply that was purchased from a provider that is not approved by Canada Life may be declined. Contact Canada Life if the item is not listed in this guide.
Basic services
Basic dentistry is comprised of routine services available in the office of a general practicing dentist that are necessary to restore teeth to natural or normal function.
Diagnostic services
Procedures conducted to determine or diagnose the dental treatment required, including:
- Standard oral examinations
- Specific oral examinations
- X-rays (including panoramic x-rays once every five years)
- A specific oral examination will be reimbursed once for any specific area and only if a standard oral examination hasn't been reimbursed within the previous 60 days
- A complete oral examination will be reimbursed to a maximum of once every three years, but not if the plan has reimbursed for any examination during the preceding nine months
Preventative services
Procedures that prevent oral disease, including:
- Cleaning and polishing teeth
- Scaling
- Topical fluoride: once every nine months
- Pit and fissure sealants, preventative restorative resins
- Fixed space maintainers intended to maintain space and regain lost space, but not to obtain more space
Restorative services
- Fillings: amalgam fillings and composite (white) fillings on all teeth. Specialty fillings and crowns such as synthetic porcelain, plastic, composite resin, stainless steel and gold may result in additional cost to be paid by the employee or dependant
- Stainless steel crowns on primary and permanent teeth
- Inlays and onlays
Only one inlay, onlay or other major restorative service involving the same tooth will be covered in a five year period.
Surgical services
All necessary procedures for extractions and other surgical procedures necessary for the treatment of disease of the soft tissue (gum) and the bones surrounding and supporting the teeth.
Endodontics
Treatment of diseases of the pulp chamber and pulp canal; including, but not limited to, basic root canal.
Periodontal services
Treatment of diseases of the soft tissue (gum) and bones surrounding and supporting the teeth, including occlusal adjustment, root planing, gingival curettage and scaling.
Replacement and repairs
- The repair of fixed appliances and the rebase or reline of removable appliances (may be done by a dentist or by a licensed dental mechanic). Relines will only be covered once per 24-month period
- With crowns, restoration for wear, acid erosion, vertical dimension and/or restoring occlusion is not covered. Check with Canada Life before proceeding
- Temporary procedures (for example: while awaiting repair of an appliance) are not covered
Recall check-up schedule
For dependent children under 19 years of age, general recall services (oral exam, polishing, scaling and fluoride) are covered once every six calendar months.
For adults and students covered under the dental plan, age 19 and older, these services are covered once every nine calendar months.
Major services
Major services apply to services required for reconstruction of teeth and for the replacement of missing teeth (for example: crowns, bridges and dentures), where basic restorative methods cannot be used satisfactorily. To determine how much of the cost will be paid by the plan, and the extent of your financial liability, you should submit a treatment plan to Canada Life for approval before treatment begins.
Reimbursement
Major services are 65% covered to plan limits. Only one major restorative service involving the same tooth will be covered in a five year period.
Restorative services
- Veneers
- Crowns and related services
- Specialty crowns and fillings, such as synthetic porcelain plastic, composite resin, stainless steel and gold may result in additional cost to be paid by the employee or dependant
Fixed prosthetics
Bridgework to artificially replace missing teeth with a fixed prosthesis.
Removable prosthetics
- Full upper and lower dentures or partial dentures of basic standard design and material
- Full dentures can be provided by a dentist or a licensed dental mechanic
- Partials can only be provided by a dentist
No benefit is payable for the replacement of lost, broken or stolen dentures.
Broken dentures can, however, be repaired under basic services.
Replacement and repairs
Removal, repairs and re-cementation of fixed appliances.
Plan limits
A dentist may charge more for services than the amount set in the governing schedule of fees or may offer to provide services more frequently than provided for in the fee guide.
You're responsible for any financial liability resulting from services performed which are not covered, or that exceed the costs covered by the plan.
Orthodontic services
This plan is designed to cover orthodontic services provided to maintain, restore or establish a functional alignment of the upper and lower teeth. The plan will reimburse orthodontic services performed after the date coverage begins.
Pre-approval
To claim orthodontic benefits, Canada Life must receive a treatment plan (completed by the dentist or orthodontist) before treatment starts.
Reimbursement
Orthodontic services are 55% covered.
The total lifetime maximum payment for orthodontic services, for each covered person, is $3,500.
The carrier will pay benefits monthly. Photocopies of receipts, as treatment progresses, must be submitted monthly (do not hold receipts until the treatment is complete). You can submit monthly claims through My Canada Life at Work.
If you pay the full amount to the dentist in advance of completed treatment, the carrier will prorate benefit payment over the months of the treatment period.
No benefit is payable for the replacement of appliances which are lost or stolen.
Treatment performed solely for splinting is not covered.
Dental general limitations
No benefits will be paid for:
- Expenses that private benefit plans are not permitted to cover by law
- Services or supplies the person is entitled to without charge by law or for which a charge is made only because the person has coverage under a private benefit plan
- Services or supplies that do not represent reasonable treatment
- Services or supplies associated with treatment performed for cosmetic purposes only
- Services or supplies associated with congenital defects or developmental malformations in people 19 years of age or over, except orthodontics
- Services or supplies associated with temporomandibular joint (TMJ) disorders
- Services or supplies associated with vertical dimension correction
- Services or supplies associated with myofascial pain
- Expenses arising from war, insurrection or voluntary participation in a riot
- Services or supplies covered under this plan’s healthcare benefit, unless the amount payable for the same expense is greater under this benefit provision
Any other item not specifically listed as being covered under this plan is not an eligible item under this dental plan.
Overview
Canada Life [Policy 6878GL(4)] administers your life insurance plan on behalf of your employer. This life insurance plan pays a benefit to your designated beneficiary, or to your estate, in the event of your death. Coverage is effective 24 hours a day, 7 days a week. This policy is a term life insurance policy and has no cash value.
Features of the plan include:
- Employee Basic Life Insurance
- Accidental Dismemberment & Loss of Sight Benefit
- Advanced payment for terminally ill employees
- A funeral advance option for the beneficiary
- A conversion policy
- Option to purchase other optional life insurance plans which includes:
- Optional Family Funeral Benefit
- Employee Optional Life Insurance
- Spouse Optional Life Insurance
- Child Optional Life Insurance
- Employee Optional Accidental Death & Dismemberment Insurance
- Spouse Optional Accidental Death & Dismemberment Insurance
- Child Optional Accidental Death & Dismemberment Insurance
Details to consider
- Do you have a spouse and/or dependents?
- Do you have other life insurance policies?
- What are your family’s financial needs?
The importance of designating a beneficiary
Life insurance payments are non-taxable when paid to one or more designated beneficiaries, and only a named beneficiary can apply for the funeral advance.
If paid to an employee’s estate, the insurance becomes part of the proceeds of the estate and may become taxable. In addition, the benefit payment is subject to probate and can be used to pay outstanding debts, taxes and other estate costs.
It generally takes longer for the benefit to be paid out through the estate.
It's highly recommended that you nominate one or more beneficiaries for your life insurance during your initial enrolment, and that you keep your beneficiary designation up to date (for example: if you get married/divorced, or if you have children).
The Benefit Service Centre must receive the original Group Life Beneficiary Designation form (PDF, 174KB) before they can update your beneficiary. If they don't receive the original form, the beneficiary will default to your estate unless you have previously designated a beneficiary, which will then remain on file.
The original Group Life Beneficiary Designation form that has been submitted with the most current date will be considered the valid form on file.
Changes in insurance
All increases and additions of new insurance coverage are subject to the actively-at-work requirement except for changes in insurance due to changes in earnings that take effect when the employee is on a Short-Term Illness and Injury Plan (STIIP), or weekly indemnity. Additions to and increases in coverage are subject to approval by the benefits carrier, which makes the determination based on the medical evidence (evidence of insurability) a requirement.
Converting to an individual plan
If your employment ends, or you reach age 65, you can apply to convert to an individual life insurance plan. Refer to the 'When does coverage end?' section for more information.
Employee Basic Life Insurance (to age 65)
Employee Basic Life Insurance is mandatory until you turn 65. No enrolment is necessary; you're automatically covered when you meet eligibility requirements.
Except as noted, coverage is equal to three times the annual salary, or the employer-paid minimum coverage ($100,000), whichever is greater.
Annual salary is defined as your bi-weekly salary times 26.0893, and coverage is rounded up to the nearest $1,000.
Important information
For nurses hired before May 1, 1990: Coverage equals 2 times annual salary rounded up to the nearest $1,000, with an employer-paid minimum of $40,000 unless the plan member elected the higher level of coverage (outlined above). For more information, refer to articles 25.04 and 27.17 of the BCNU Collective Agreement.
For employees working past age 65: Employee Life Insurance (and long-term disability) will cease at the end of the month in which an employee turns 65. Employees have the option to convert their group life insurance plan to an individual plan. See 'When does coverage end?' for more information and important application deadlines.
For employees who retire before age 65: Employee Life Insurance will continue until the age of 65 provided that:
- While an employee, the retiree was covered under the Public Service group life insurance plan (Policy 6878)
- The retiree begins receiving a pension the month following termination of employment AND elects (on their pension application form) to continue life insurance coverage (the coverage amount is what it was on the day before they retire). Those under 65 will be provided with this option (see your pension package)
You are not eligible for this coverage if there has been a break in service from the end of employment to the commencement of your pension payment
Premiums
The premium for the first $100,000 of insurance coverage is paid by your employer and is a taxable benefit. The employee-paid monthly premium for coverage above $100,000 is nine cents per thousand dollars (rate subject to change) and is paid through payroll deduction.
Limitations
There are no limitations or restrictions on employee basic life claims for eligible employees under age 65 or eligible retired employees under age 65, except as under accidental dismemberment and loss of sight.
Other benefits included in the Employee Basic Life Insurance plan
Accidental Dismemberment & Loss of Sight
If you suffer one of the following losses as a result of an accident, you'll receive 100% of the principal sum for:
- Loss of both hands or both feet
- Loss of sight of both eyes*
- Loss of one hand and one foot
- Loss of one hand or one foot and sight of one eye*
If you suffer one of the following losses, you'll receive 50% of the principal sum for:
- Loss of one hand or one foot
- Loss of sight of one eye*
*Loss of sight means total and irrevocable loss beyond correction by surgical or other means.
If benefits are paid to you because of an accidental dismemberment or loss of sight benefit claim, and you die as a result of that injury, the payment to your beneficiary will be reduced by the benefit payment you received before your death.
A claim for accidental dismemberment or loss of sight should be made in writing as an AskMyHR (IDIR restricted) service request using the categories Myself (or) My Team or Organization > Benefits > Bargaining Unit Employees. Forms and instructions will be forwarded for you and your physician to complete.
Advance payment for terminally ill employees
If you're suffering from a terminal illness with a life expectancy of 24 months or less, you may be eligible to receive an advance payment of up to $50,000 or 50% of your Employee Basic Life Insurance, whichever is less. This payment is non-taxable.
Contact MyHR to make a claim and provide them with the following information:
- Full name
- Social insurance number
- Current address
- Telephone number
- Last day worked
- Work status
The remaining portion of your Employee Basic Life Insurance will be paid to your designated beneficiary upon your death. Interest payments will be charged against the advance payment.
Funeral advance
An advance of $10,000 can be expedited to the beneficiary in the event of an employee’s death. This doesn't apply if the estate or a minor child has been designated as the beneficiary. The balance of the Employee Basic Life Insurance will be paid once the beneficiary has submitted the claim.
To apply for the funeral advance, the beneficiary should contact MyHR and provide the following information:
- Name of deceased person
- Date of birth of deceased person
- Date of death of deceased person
- Full name, address and phone number of beneficiaries
After confirming that the funeral advance is payable, the Benefits Service Centre will contact the carrier and a cheque will be mailed directly to the beneficiary, usually within a few days of the request.
Optional life insurance plans
Additional life insurance is available to you if you want to supplement your Employee Basic Life Insurance and/or if you wish to insure any of your dependents. All Optional Life and Optional AD&D coverage for yourself or your spouse ends when the covered individual turns 65.
Employee Optional Life Insurance
This optional plan provides employee life insurance in addition to employee basic life insurance. You may select insurance in units of $25,000 up to a maximum of $1 million. The beneficiary of this coverage is the same as designated for basic life insurance unless otherwise specified.
Spouse Optional Life Insurance Benefit
This optional plan provides life insurance for your spouse. You may select insurance in units of $25,000 up to a maximum of $500,000. You are the beneficiary of the life insurance.
Child Optional Life Insurance Benefit
This optional plan provides life insurance for any/all dependent children you choose to cover. Evidence of insurability is not required, and you may select insurance in units of $5,000 up to a maximum of $20,000. You are the beneficiary of the life insurance.
Initial enrolment
During initial enrolment, you can select up to $50,000 of Employee Optional and/or Spouse Optional Life Insurance coverage without providing evidence of insurability. Any amount over $50,000 during initial enrolment will require evidence of insurability.
After initial enrolment, if you wish to increase your or your spouse’s life insurance coverage, you'll be required to provide an evidence of insurability form to the carrier.
When submitting your Evidence of Insurability form, please ensure to include the division number for BC Public Service employees covered under the Bargaining Unit Benefits Plan (Division 40).
Applications must be approved before coverage can begin.
Waiver of premium benefit on optional life insurance
If you become disabled while insured, the insurance carrier will review whether you're eligible for a premium waiver on the optional life insurance for yourself and your covered dependents throughout the benefit period. Waiver of premium will continue during the period that you're continuously disabled but will not continue beyond your 65th birthday.
Suicide limitation on optional insurance
Optional employee and optional spouse life insurance benefits are not paid if the insured person (you or your spouse) commits suicide within two years after optional life insurance takes effect or increases. The beneficiary will receive a refund of the premiums paid for that insurance.
Optional Family Funeral Benefit plan
This optional plan provides spousal coverage of $10,000 and coverage of $5,000 per dependent child. The beneficiary of this coverage is the employee. The premium is $2.16 per month (rate is subject to change), regardless of the number of dependents. Evidence of insurability is not required.
Optional Accidental Death & Dismemberment Insurance (AD&D)
AD&D insurance is available to supplement your Employee Basic Life Insurance coverage and/or to cover any of your dependents as a result of accidental death or the loss of use of limbs, sight, speech, or hearing. This benefit doesn't provide coverage due to illness. Coverage is provided 24 hours a day, 7 days a week. Evidence of insurability is not required.
Three plans are available:
Employee Optional AD&D
You may select insurance in units of $25,000 up to a maximum of $500,000.
Spouse Optional AD&D
You may select insurance in units of $25,000 up to a maximum of $500,000.
Child Optional AD&D
You may select insurance in units of $10,000 up to a maximum of $250,000.
The beneficiary of this coverage is:
- In the event of employee’s death: the same as designated for employee basic life insurance unless otherwise specified
- In the event of spouse’s or child’s death: the employee
- In the event of eligible injury to employee: the employee
- In the event of eligible injury to spouse or child: the employee
Important definitions regarding loss
Loss by dismemberment means:
- For hands and feet, complete severance through or above the wrist or ankle joints
- For arms and legs, complete severance through or above the elbow or knee joints
- For thumb and big toe, complete severance of one entire phalange
- For fingers and other toes, complete severance of two entire phalanges
Loss of sight, speech and hearing means total and irrecoverable loss beyond correction by surgical or other means.
Loss of use means total and irrecoverable loss of the ability to perform every action the arm, leg or hand was able to perform before the accident occurred, beyond correction by surgical or other means. Benefits will not be paid for loss of use of the same arm, leg or hand for which loss by dismemberment is paid.
Eligible injuries
AD&D insurance will pay a percentage of the insurance to you if you sustain certain injuries in an accident. Eligible injuries usually involve dismemberment (loss of a limb, toe or finger) or permanent loss of use, such as paralysis or vision loss.
Benefits
The amount of AD&D insurance you purchase is called the principal sum. For example, if you purchase two units of $25,000 for yourself, your principal sum is $50,000. If you purchase three units of $25,000 for your spouse, your spouse’s principal sum is $75,000.
Depending on the loss you, your spouse or your child suffers as a result of an accident, a percentage of the applicable principal sum is paid as per the table of losses below if any of the following occur within 365 days of the accident.
| For loss of | Amount payable |
|---|---|
| Life | The principal sum |
| Both hands | The principal sum |
| Both feet | The principal sum |
| Sight of both eyes | The principal sum |
| One hand and one foot | The principal sum |
| One hand and sight of one eye | The principal sum |
| One foot and sight of one eye | The principal sum |
| Speech and hearing in both ears | The principal sum |
| One arm | 3/4 of the principal sum |
| One leg | 3/4 of the principal sum |
| One hand | 1/2 of the principal sum |
| One foot | 1/2 of the principal sum |
| Sight of one eye | 1/2 of the principal sum |
| Speech | 1/2 of the principal sum |
| Hearing in both ears | 1/2 of the principal sum |
| Thumb and index finger | 1/4 of the principal sum |
| Four fingers of one hand | 1/4 of the principal sum |
| All toes of one foot | 1/8 of the principal sum |
| For loss of use of | Amount payable |
|---|---|
| Both arms and legs (quadriplegia) | 2x the principal sum |
| Both legs (paraplegia) | 2x the principal sum |
| One arm and one leg on same side of body (hemiplegia) | 2x the principal sum |
| One arm and one leg on different sides of body | The principal sum |
| Both arms | The principal sum |
| Both hands | The principal sum |
| One hand and one leg | The principal sum |
| One arm | 3/4 of the principal sum |
| One leg | 3/4 of the principal sum |
| One hand | 1/2 of the principal sum |
Surgical reattachment
50% of the dismemberment benefit is payable if a dismembered part is surgically reattached regardless if use is regained. The balance of the dismemberment benefit is paid if the reattachment fails and the reattached part is removed within one year after the reattachment is performed.
Other benefits
If benefits are payable under this plan for a covered accident, there may be other benefits paid to plan maximums in addition to loss of life, dismemberment or loss of use benefits.
- If death occurs 150 kilometres or more from home, up to $2,500 will be paid for preparation of the body and transportation to its burial place or crematory. This benefit is also available to your dependents under the family plan
- If your death is accidental, your spouse may be reimbursed for an occupational training program. The maximum amount payable is the lesser of:
- 10% of the principal sum; and
- $10,000
- If your death is accidental, your child or children may be reimbursed for tuition if they enrol as a full-time student at a post-secondary institution. Canada Life will pay the educational benefit each year for a maximum of four consecutive years upon receipt of proof of full-time enrolment. If the child was enrolled as a full-time student at a post-secondary institution at the time of the accident or if the child was enrolled as a full-time student at a secondary school at the time of the accident and enrols at a post-secondary institution within 365 days of the accident. The maximum amount payable for each year of full-time post-secondary school enrolment is the lesser of:
- 5% of the principal sum; and
- $5,000
- Up to $2,000 for transportation and lodging expenses to have one family member join the covered person if they're hospitalized more than 150 kilometres from their home
- Fees for an employee or their spouse to enrol in an education program if a job change is required because of an accident
- Must enrol at a post-secondary institution within 365 days after the accident
- Maximum payable is $10,000
- Expenses to make the covered person’s house and vehicle wheelchair accessible
- Expenses incurred must be within 365 days of the accident
- Maximum amount payable for all home and vehicle modifications combined is $10,000
For more information on the limitations and specifications related to these additional benefits, please contact MyHR or submit an AskMyHR (IDIR restricted) service request. Use the categories Myself (or) My Team or Organization > Benefits > Bargaining Unit Employees.
Accidental Dismemberment & Loss of Sight coverage and Optional Accidental Death & Dismemberment coverage limitations
No benefits will be paid for loss resulting from or associated with the following:
- Suicide, regardless of state of mind
- Intentionally self-inflicted injury, regardless of state of mind
- Viral or bacterial infections, except pyogenic infections occurring through the injury for which loss is being claimed
- Disease or critical illness
- Medical or surgical treatment other than reattachment
- Service (including part-time or temporary service) in the armed forces of any country
- War, insurrection or voluntary participation in a riot
- Air travel, except as a passenger in a licensed aircraft flown by a pilot certified to fly the aircraft. No benefits will be paid where the aircraft is owned, leased or rented by the Province of B.C., or where the person who suffers the loss is acting as a crew member
- Participation in a criminal act or attempted criminal act
This section provides you with the methods to make an extended health, drug, dental or life insurance claim.
My Canada Life at Work
My Canada Life at Work is Canada Life's self-service website for your extended health and dental plans.
- Submit eClaims
- Update direct deposit banking information
- View your coverage at a glance
- Track your eligibility and limits
- View or print ID cards
Benefits ID cards are no longer being mailed to plan members but can be accessed online through My Canada Life at Work.
Once your benefits are active, log into Employee Self Service (ESS) to view your Canada Life Policy (50088) and ID number.
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
My Time and Pay > Employee Self Service >Benefit Summary > Extended Health/Dental
You will require the policy number and ID number to register for access to My Canada Life at Work.
Please allow three to five business days after your benefits are in effect to register. You can also download the My Canada Life at Work Mobile app to your devices.
If you have problems registering for My Canada Life at Work, please call Canada Life.
Most claims can be submitted online, but there are some claims that require members to complete a specific claim form. These paper claim forms and receipts can be uploaded on My Canada Life at Work so members don't have to mail them to Canada Life.
Members can upload a photocopy, scan or picture of their claims by logging into My Canada Life at Work and going to Make a claim > Start other claim to submit the following claims types:
- Medical travel
- Estimates of what Canada Life will cover (predeterminations)
- Other health, dental, drug and HSA claims that cannot be submitted using My Canada Life at Work’s regular 'Make a claim' process
- Claims older than 12 months that normally would be submitted through online claims
Out of country claim forms are available on My Canada Life at Work and can be submitted online to Global Excel, by email to canadalife.claims@globalexcel.com or by mail following the instructions on the claim form.
Please ensure that your address is updated with your employer. Once your address is updated with your employer, it will be updated with Canada Life.
If you have access to Employee Self Service (ESS), you can update your address online.
My Time and Pay > Employee Self Service > Personal Details
- Time and Leave: access from work (IDIR restricted)
- Time and Leave: access from home (IDIR restricted)
If you don't have access to ESS, call MyHR (1-877-277-0772) and a Service Representative will be able to update your information in PeopleSoft.
Pay Direct
Pharmacies, dentists, chiropractors, physiotherapists, naturopathic doctors, podiatrists, psychologists, massage therapists and optical stores/optometrists/ophthalmologists can register for Pay Direct through Canada Life.
If your service provider has signed up, simply provide them with your policy and ID number (and those for your spouse’s program, if you can coordinate benefits) and you will pay only the portion of the expense that's not covered under your benefits plan(s).
Extended health and drugs
To make a claim for reimbursement, you can submit a paper or electronic claim.
- Find the paper claim form on the Careers & MyHR forms and tools index page or My Canada Life at Work, and follow the submission instructions carefully. Make a photocopy of your expense receipt because the originals will not be returned to you.
- Submit eClaims on My Canada Life at Work for prescription drugs, vision care, chiropractic, physiotherapy, podiatry, psychology, acupuncture, massage therapy and naturopathy. Keep your original expense receipts in case you're asked to submit them.
Once a claim is processed, you’ll receive a direct deposit if you’ve provided your banking information to Canada Life through My Canada Life at Work, otherwise you will receive a cheque in the mail.
All plan members are required to sign up for PharmaCare to assist with prescription drug coverage, limiting the impact on your lifetime maximum. In addition, some high-cost drugs will require you to apply for PharmaCare special authority before you can be reimbursed.
For information regarding drugs and medicines, please refer to the Extended health plan section.
Out of country emergency medical travel claims
Out of country claim forms are available on My Canada Life at Work and can be submitted online to Global Excel, by email to canadalife.claims@globalexcel.com or by mail following the instructions on the claim form.
Dental
Most dental offices will bill Canada Life directly when you provide your policy and ID number (and your spouse’s information, if you have coordinated benefits) and you'll pay only the portion of the service not covered by your benefits plan(s).
If your dentist cannot bill Canada Life directly (meaning you have to pay the full cost at the dental office), you can submit a paper claim
Find the paper claim form on the Careers & MyHR forms and tools index page, or My Canada Life at Work, and follow the submission instructions carefully. Make a photocopy of the expense receipt because the originals will not be returned to you.
Monthly orthodontic claims may be claimed through My Canada Life at Work.
Deadlines
It's recommended that you submit claims immediately after treatment.
Late claims will not be accepted by Canada Life.
Extended health claims, including drug claims and dental claims, must be received no later than 15 months from the date the expense was incurred.
For all claims questions, contact Canada Life at 1-855-644-0538.
Life insurance
To initiate a claim for any of the life insurance products, you, your supervisor or your designated beneficiary can contact MyHR.
To submit an AskMyHR (IDIR restricted) service request, use the categories Myself (or) My Team or Organization > Benefits > Bargaining Unit Employees.
A representative will send claiming information and will be available to answer your questions.
Coordination of benefits
If your spouse is a BC Public Service employee and is covered under the BC Public Service benefits plan (excluding BC Ferries plan members), you're able to coordinate benefits and submit your extended health and dental receipts to both plans and get up to 100% of your eligible expenses reimbursed (to plan limits).
If your spouse is enrolled in a benefits program with an employer outside of the BC Public Service, check your spouse’s benefits program to see if it allows for coordination of benefits plans.
Insurance companies follow the guidelines below to determine which plan pays first and how benefits are calculated.
- When you make a claim under coordinated plans, photocopy your receipt(s) and submit your claim to your plan first
- Once approved, you'll receive an Explanation of Benefits Statement. Now you can submit a claim to your spouse’s plan, along with the Explanation of Benefits Statement and photocopies of your receipt(s)
- Spouses will submit to their plan first, and to your plan second
- If you have dependent children, the order of submission is determined by your birthdays. If your birthday is earlier in the calendar year than that of your spouse, you'll submit your children’s claims to your program first
If you and your spouse have coordinated benefits and you're both covered under Canada Life, you can submit to both plans at the same time by filing an eClaim through My Canada Life at Work.
If not, you can submit an extended health claim form or a dental plan claim form which you can find on the Careers & MyHR > Forms and Tools > For All Employees page or My Canada Life at Work.
When coordinating benefits, please ensure the same names are being used on both plans (for example: legal names) so there are no delays with the coordination of benefits with the carrier. If the names don't match, there may be a delay in payment or payment may be missed.
Once your claim is processed, you'll receive notification. If you provided Canada Life with your bank information, they’ll deposit the reimbursement into your bank account; otherwise, you'll receive a cheque in the mail.
A retiree plan will always pay after any group plan that covers you as an employee.
Work status changes
The BC Public Service recognizes that each of us, throughout our career in the BC Public Service, may experience various work events (for example: becoming a new employee, travelling out of the country, leaving the public service, etc.) that will change the type of coverage we receive.
The following is a list of common work status changes and the effects on benefits coverage.
If you have any questions, contact MyHR.
If submitting an AskMyHR (IDIR restricted) service request, use the categories Myself (or) My Team or Organization > Benefits > Bargaining Unit Employees.
| Question |
Answer |
|---|---|
| I transfer from a regular position to an auxiliary position? |
Your benefits coverage ends at the end of the month of your date of transfer and you must re-qualify for benefits. |
| I'm on a temporary assignment to an excluded position from a base position in the bargaining unit position? |
If your temporary assignment is 21 days or longer, you're eligible (and can enrol) for the benefits program available to excluded employees. You become eligible on the first day of the month following the start of your temporary assignment to the excluded position. More information about benefits for excluded employees (Flexible Benefits Program) is available on Careers & MyHR. If you return to your base position, you return to your bargaining unit benefits program. If you allocated funds to a Health Spending Account, it terminates at the end of the month you return to your base position. The remaining balance is forfeited. If you're enrolled in any of the Optional Life Insurance Plans, your coverage transfers between the two benefit plans. A change in employment is not considered an eligible life event, therefore no changes can be made to your life insurance coverage as a result of a job change. Your extended health and dental claims history remain with you throughout your employment. You should always check your eligibility prior to purchase. |
| I transfer to an excluded position? |
You become eligible (and can enrol) for the benefits program available to excluded employees. Refer to the 'Who’s eligible for benefits?' section on the Benefits for Excluded employees page on Careers & MyHR. If you do not enrol, you will be enrolled (by default) in the benefit plans that most closely match your coverage under the Bargaining Unit Benefit Plan. Any dependents covered under the Bargaining Unit Benefit Plan will also be covered under the Flexible Benefits Program. Any unused flex credits will be paid out in monthly instalments as taxable cash. You will have to wait until the next Open Enrolment period (or until you experience an eligible life event) to make any changes. If you're enrolled in any of the Optional Life Insurance Plans, your coverage transfers between the two benefit plans. A change in employment is not considered an eligible life event, therefore no changes can be made to your life insurance coverage as a result of a job change. Your extended health and dental claims history remain with you throughout your employment. You should always check your eligibility prior to purchase. |
| I'm on Short Term Illness and Injury Plan (STIIP)? |
There are no changes to coverage. |
| I'm approved for Long Term Disability (LTD)? |
There are no changes to coverage. |
| I commence a rehabilitation trial? |
If you return to work on a rehabilitation trial after being on LTD, your LTD claim continues to be active, and there are no changes to coverage. |
| I return to work from Long Term Disability (LTD)? |
There are no changes to coverage. |
| I'm on leave with pay? |
There are no changes to coverage. If you're on a leave with partial pay, visit the Benefits while on leave or layoff page on Careers & MyHR for detailed information. |
| I'm on leave without pay? |
Benefits coverage is suspended during a leave without pay over 1 calendar month, but you can continue to receive benefits coverage by paying the full cost of the plan premiums. If your leave is more than 30 days but less than 90 days and you do not maintain your optional life insurance benefits, your optional life insurance coverage will be reinstated upon your return to work. If your leave is more than 90 days and you don’t maintain your optional life insurance benefits, any optional coverage for which evidence of insurability is not required will be reinstated but you’ll need to requalify and provide evidence of insurability for Employee Optional and/or Spouse Optional Life Insurance. If the leave is included in Part 6 of the Employment Standards Act, your benefits, other than Optional Life Insurance plans, are continued. Review the Benefits while on leave or layoff page on Careers & MyHR for detailed information. |
| I return from a leave without pay? |
If your leave is under three months, contact MyHR when you return to reinstate your benefits. Submit an AskMyHR (IDIR restricted) service request using the categories Myself (or) My Team or Organization > Benefits > Submit a Health Benefit Form/Application. If your leave is greater than three months, follow the enrolment process to reinstate your benefits. If your leave is more than 30 days but less than 90 days and you do not maintain your optional life insurance benefits, your optional life insurance coverage will be reinstated upon your return to work. If your leave is more than 90 days and you don’t maintain your optional life insurance benefits, any optional coverage for which evidence of insurability is not required will be reinstated but you’ll need to requalify and provide evidence of insurability for Employee Optional and/or Spouse Optional Life Insurance. |
| I'm on maternity/parental/pre-placement adoption leave? |
The birth of a child is an eligible life event and you have 60 days from the birth of your child to update your benefits coverage. You can enrol them in your benefits by submitting the Bargaining Unit Benefits Plan Enrolment/Change form (PDF, 378KB). After 60 days, you can still add your child to your coverage, but you can’t change your optional life insurance options. Benefits in place prior to your leave will remain in place during the leave. If you choose, you may waive extended health and dental plan coverage during your leave by completing and submitting the Bargaining Unit Benefits Plan Enrolment/Change form (PDF, 378KB) along with your maternity/parental leave forms. Employees often consider this option if:
Maintenance of Employee Basic Life Insurance and Long-Term Disability coverage is mandatory during the leave. If you have waived, are not eligible for or have deferred your top-up allowance, your benefits will be maintained (if you do not cancel them) but any optional life insurance plans will be cancelled. You can choose to maintain your Optional Life Insurance coverage by submitting an application and paying the premiums. If you discontinue your Optional Life Insurance, any coverage which evidence of insurability is not required can be reinstated. For example, the Optional Family Funeral Benefit can be reinstated. However, you'll need to reapply and requalify by submitting evidence of insurability for Employee Optional and/or Spouse Optional Life Insurance. More information can be found on the Careers & MyHR page, Benefits while on leave or layoff. If you're taking extended childcare leave after parental leave and would like to maintain your benefits, you'll have to pay the premiums. More information can be found on the Careers & MyHR page Benefits while on leave or layoff. After your leave, if you do not fulfil the return-to-work requirements, you'll have to repay any premiums that were paid on your behalf by your employer prior to April 1, 2022. For more information, refer to: |
| I travel out-of-province/out-of-country? |
Please see the out-of-province/out-of-country emergency coverage information in the 'Extended health plan' section of this benefits guide for detailed information on emergency medical coverage while traveling for work and/or pleasure.
|
| I'm laid off from the BC Public Service? |
Your extended health and dental coverage and life insurance plans end on the last day of the month of layoff. Benefits coverage can be continued for six months following the month of layoff if you apply to continue coverage and pay the premiums. Visit Benefits while on leave or layoff on Careers & MyHR for more information. |
| I'm actively working, and I reach the age of 65? |
There are no changes to extended health and dental. You're no longer eligible for Employee Basic Life Insurance, Optional Family Funeral Benefits or for any of the Optional Life Insurance or Optional Accidental Death & Dismemberment Insurance plans, but you can convert to an individual plan. For more information, see 'Converting to individual benefits plans' in the 'When does coverage end?' section. You're also no longer eligible for Long Term Disability. |
| I retire from the BC Public Service? |
Your coverage ends at the end of the month in which you retire. Retirement benefits are administered through the BC Public Service Pension Plan and are different then your benefits coverage through the BC Public Service. If you are under age 65, you have the option to continue your employee basic life insurance and optional family funeral benefit by applying through the Public Service Pension Plan. Review retirement benefits criteria at the BC Pension Corporation website. |
| I resign from the BC Public Service? |
Your extended health and dental coverage end on your last day of work. Your life insurance plans end on the last day of the month in which your employment ends. See 'Converting to individual benefits plans' under the 'When does coverage end?' section for further information. Benefits coverage extended to an eligible spouse and/or dependent children will end the same date that your coverage ends. |
| I die? |
Employee coverage Extended health and dental plan coverage for dependants Optional Life and Optional AD&D coverage for dependents |
Extended health and dental plans
Coverage ends on one of the following:
- Your last day of employment
- The day you request that coverage end
- The last day of the month of a leave of absence without pay greater than a calendar month (if you don't pay the required premiums)
- The last day of the month in which you change from regular to auxiliary status
- The last day of the month of lay off (if you don't pay the required premiums)
- The last day of the month in which you're on pay prior to retirement
Employee Basic Life and Optional Family Funeral Benefit
Coverage ends on the date the policy terminates or the last day of the month in which any of the following occurs:
- Your employment ends
- You turn 65
- You change from regular to auxiliary status
- You retire under the provisions of the Public Sector Pension Plans Act (unless you elect to continue coverage to age 65)
- After the month in which a premium is not received by you or your employer on your behalf
- You cease to satisfy the actively-at-work requirement
Optional Life and Optional AD&D Insurance
Coverage ends on the date the policy terminates or the last day of the month in which any of the following occurs:
- Your employment ends
- You turn 65
- You change from regular to auxiliary status
- You retire under the provisions of the Public Sector Pension Plans Act
- After the month in which a premium is not received by you or your employer on your behalf
- You cease to satisfy the actively-at-work requirement
Coverage for eligible dependents
Coverage for eligible dependents ends on one of the following:
- The same date that your coverage terminates
- The date you request coverage end
- The date they cease to qualify as an eligible dependent
- For Spouse Optional Life and Spouse Optional AD&D, the date that the spouse turns 65
- In the event of the employee’s death, extended health and dental plan coverage for dependants is maintained until the end of the month following the month of the employee’s death
When your spouse turns 65, they're eligible to convert to an individual life insurance plan without a medical exam. See the heading 'Converting your spouse’s optional life insurance' in this section for further details.
Converting to individual benefits plans
The conversion policy enables you to convert to individual extended health, dental and life insurance plans when your group coverage ends.
Converting to an individual plan may benefit you if you don't qualify for other insurance due to an existing medical condition.
You can apply to convert to some or all these plans.
You must apply and pay your first premium within 60 days of the end of the month in which your group coverage ends.
This conversion cannot be made retroactive. If you miss this deadline, you're no longer eligible for conversion.
Converting your individual life insurance plans
If your employment ends or you reach age 65 (and are no longer eligible for group life insurance), you may convert your coverage to an individual policy, limited in both amount and plan, without a medical examination. Or, you may take a medical examination (paid for by the carrier) and choose any insurance plan offered by the company. If you don't meet the medical requirements, you can still convert your coverage to an individual policy, limited in both amount and plan.
The amount of the individual policy where no medical examination is taken may be any amount up to the amount of coverage combined (maximum $200,000) in force at the time your group coverage ends. The premium for the individual policy will depend on your age and on the type of policy you select. It's not the same rate as paid while covered under the group plan.
For employees turning 65, you'll be provided instructions from the Benefits Service Centre on how to start the conversion process. For employees who are terminating their employment before turning 65 and who reside in British Columbia, you can apply to Canada Life for an individual policy by contacting Todd Prystupa at 250-217-0751. For employees who reside outside of B.C., please visit the Canada Life Group Life Conversion page to find an adviser in your area, or call 1-888-252-1847.
Please provide the following notes to the adviser you’re working with:
- The combined conversion maximum is $200,000
- A plan member must apply for the individual policy in writing and pay the first premium within 60 days after the life insurance terminates
- The actual amount of life insurance that's eligible for conversion, as well as the employee’s termination date, will be verified upon receipt of the conversion application at Canada Life’s Head Office. The verification will be between Canada Life Head Office and the Plan Member’s HR/Payroll Office
Converting your spouse’s optional life insurance
Provided your spouse is under age 65, you may also convert their optional life insurance to an individual plan at the same time as you are converting your own coverage. The same application deadline and process to convert coverage applies.
If your spouse is older than you when you turn 65, your spouse is ineligible for conversion to an individual plan.
Individual extended health and dental plans
When your group coverage ends, an individual health and dental plan is available through Canada Life. Visit the Canada Life Health and Dental Insurance page for more information.
If you would like to purchase an individual extended health and dental plan, contact Canada Life.
Individual plans will be different than the group plan.
You're free to apply for insurance with any other insurance carrier you choose at any time. MyHR, the Public Service Pension Plan at BC Pension Corporation and your employer are not responsible for the lapse of the 60-day conversion period if you don't apply in a timely manner.
Glossary
| Term | Definition |
|---|---|
| Actively-at-work requirement |
To satisfy this requirement, an employee must:
|
| Annual earnings | For the purposes of Employee Basic Life Insurance, annual earnings are defined as 12 times your current monthly base rate of pay for your current classification, calculated as bi-weekly salary times 26.0893. Annual earnings are the employee’s basic annual salary paid by the employer, including salary protection, classification adjustments, and some temporary market adjustments. Overtime, allowances, bonuses or any other additions to pay are not included. |
| Annual enrolment (Optional Life Insurance plans) | Annual enrolment period where you can update your optional life insurance choices, with changes taking effect April 1 of the current calendar year. |
| Auxiliary employee | An employee who is employed for work that is not of a continuous nature. Refer to your Collective Agreement for information on eligibility requirements for benefits. |
| Bargaining unit employee |
The bargaining unit consists of those public service employees who are members of one of the following bargaining units:
|
| Beneficiary |
The person(s)/registered charity named to receive the insurance benefit if the employee dies while insured. If the employee dies without designating a beneficiary, payment will be made to the employee’s estate. The employee is the beneficiary for Spouse Optional and Child Optional Life Insurance. |
| Carrier |
The service provider that adjudicates the claims on behalf of the employer:
|
| Claim | A request to the insurance provider for payment under the benefits plan. |
| Common-law spouse |
A common-law spouse is a person of the same or opposite sex where the employee has signed a declaration or affidavit that they have been living in a common-law relationship or have been cohabiting for at least 12 months. The period of cohabitation may be less than 12 months where the employee has claimed the common-law spouse’s child/children for taxation purposes. By enrolling your common-law spouse in your benefits program, you're declaring that person as your common-law spouse. A separate form (declaration) is not required. |
|
Complete oral exam |
Clinical examination and diagnosis of hard and soft tissues, including carious lesions, missing teeth, determination of sulcular depth and location of periodontal pockets, gingival contours, mobility of teeth, recession, interproximal tooth contact relationships, occlusion of teeth, TMJ, pulp vitality tests, where necessary and any other pertinent factors. |
|
Conversion policy |
A policy that enables members to convert to individual benefits plans (extended health and dental, life insurance) when group coverage ends. |
|
Coordination of benefits |
A provision in a group insurance policy describing which insurer pays a claim first when two policies cover the same claim. This provision applies only to extended health and dental plans. Under this provision, the total benefit amount that an individual can claim is 100% of the cost of the eligible expense incurred (meaning the combined reimbursements across all plans cannot exceed the total cost of the expense). |
|
Deductible |
The amount you must pay each year before the plan starts to reimburse eligible medical expenses. |
|
Dependants |
A spouse or child who meets the eligibility requirements and is covered under your benefits program. |
|
Dispensing fee |
The fee charged by pharmacies to dispense a medication. |
|
Eligible employee |
All regular bargaining unit employees, whether full or part-time, may participate in this benefits program. In addition, auxiliary bargaining unit employees may participate in this benefits program upon meeting eligibility criteria (for example: completion of 1,827 hours of work in 33 pay periods). See your collective agreement for additional information about eligibility criteria. |
|
Eligible expenses |
Charges for services and/or supplies that have been specifically included in the Extended Health and Dental Contract as a benefit. An expense is incurred on the date the service is provided or the supply is received. Any payment to a pharmacy or practitioner which represents an amount more than the recognized fee schedules is not included in the definition of an eligible expense. |
| Eligible life event | A specific event or change that allows you to make changes to your optional life insurance plans within 60 days of the event. Eligible life events include events such as a birth or death of a dependent, a change in marital status, or the loss of a spouse’s benefits coverage. |
|
Employer |
BC Public Service or an employer participating in the public service benefits program. |
|
Estate |
The whole of one’s possessions (assets and liabilities) left by an individual upon their death. |
| Evidence of Insurability | The documentation of the good health to be approved for Employee and Spouse Optional Life Insurance. This is also called 'evidence of good health.' |
|
Explanation of benefits statement |
The statement you receive from your extended health/dental insurance carrier that itemizes how you're being reimbursed for the expenses that you submitted. |
|
Fee schedule |
The dental fee schedule published by the BC Dental Association for dentists (general practitioners), dental specialists, and denturists that contains eligible dental services, financial limits, treatment frequencies, and fees in effect on the date the dental service was performed. Most, but not all, plans will cover costs based on the fee guide. It's not mandatory for dental offices to follow the fees suggested in the fee guide. |
|
Full-time attendance |
A child is considered a full-time student when they meet the attendance requirements specified by the educational institution. If not specified, full-time attendance means that the child is enrolled for at least 15 hours of instruction per week, per term, and is physically present on campus OR virtually present on campus by way of regularly scheduled, interactive, course-related activities conducted online. Students must be able to demonstrate, if requested, that they meet full-time attendance requirements. |
|
Individual benefits plans |
Benefits plans that an individual purchase for themselves. |
|
Low Cost Alternative program |
Under PharmaCare, drugs deemed the lowest cost alternative are usually (but not always) generic drugs. Generic drugs contain the same active ingredients and are manufactured to the same standards set by Health Canada, and to the same strict regulations established by the Food and Drugs Act. Only minor ingredients like dyes, coatings or binding agents may vary. The real difference is in price; generic drugs cost 30 to 50% less, on average. |
|
Minor |
A person who's under 19 years of age. |
|
Non-taxable benefits |
Non-cash benefits, like extended health and dental, provided to employees by their employer. Employees are not required to pay the tax on the cash value of the benefit. |
|
Paramedical services |
A defined group of services and professions that supplement and support medical work, but don't require a fully qualified physician. These services include:
|
|
PharmaCare |
PharmaCare helps British Columbians with the cost of eligible prescription drugs and designated medical supplies. It's one of the most comprehensive drug programs in Canada, providing reasonable access to drug therapy through seven drug plans. Assistance through PharmaCare is based on income. The lower your income, the more help you receive. There's no cost to register and there are no premiums. More information is available on the PharmaCare page. |
|
Pre-authorization |
Confirmation with Canada Life regarding eligible medical/dental expenses and reimbursement percentage. |
|
Premium |
The amount paid by the employee or the employer to maintain insurance coverage. |
|
Principal sum |
An amount equal to the employee’s life insurance. |
| Qualifying disability (Optional Life Insurance only) |
An employee is considered disabled if disease or injury prevents them from being gainfully employed. Gainful employment means work:
The availability of work will not be considered in assessing disability. *Indexed annual earnings are pre-disability earnings that have been adjusted to reflect changes in the Consumer Price Index. |
|
Reasonable & Customary (R&C) limits |
Represents the standard fees health care practitioners would charge for a given service. R&C limits are reviewed regularly and are subject to change at any time. If your health care practitioner charges more than the R&C limit for that item or service, you'll be responsible for paying the difference. For R&C charges, log into My Canada Life at Work under Coverage & Balances, Health (50088), and Customary charges to view. If you have any questions about R&C limits for a given service, contact Canada Life at 1-855-644-0538. |
|
Reference-based pricing |
A process where drugs that are deemed therapeutically equivalent are grouped together, and then the cost of the lowest-priced drug in the group (typically a generic drug) is used as the reimbursement level for all drugs in the group. |
|
Regular employee |
An employee who is employed for work that is of a continuous full-time or continuous part-time nature. |
|
Rehabilitation trial |
A trial period of employment for assessment and/or rehabilitation purposes. |
|
Reimbursement |
The amount you're paid back for an expense that you incur. Reimbursements can be partial or total. |
|
Specific oral exam |
The examination and evaluation of a specific condition in a localized area. |
|
Statutory benefits |
Benefits that are fixed, authorized, or established by statute. The employer is required by the law (Employment Standards Act) of the province to provide these benefits to employees. |
|
Taxable benefits |
Non-cash benefits, like Employee Basic Life Insurance (employer’s portion) provided to employees by their employer. Employees are required to pay the tax on the cash value of the benefit. |
| Term life insurance | Life insurance protection provided during your term of employment. Term life insurance has no cash value. |
| Weekly indemnity | A benefit payable to eligible auxiliary employees who are ill and who don’t qualify for coverage under the Short-Term Illness and Injury Plan. See your Collective Agreement on Careers & MyHR for further information. |
Contacts and resources
For questions about extended health and dental claims, contact Canada Life.
Canada Life Mailing Address
PO Box 3050, Station Main
Winnipeg MB R3C 0E6
Canada Life Phone: (Toll-free) 1-855-644-0538
Assistance with My Canada Life at Work for Plan Members: (Toll-free) 1-888-222-0775
Visit Canada Life's website.
To check your benefits or to submit a claim, visit My Canada Life at Work.
Optional emergency travel medical benefits
Visit Canada Life's website.
Phone: (Toll-free) 1-800-565-4066
How to submit forms without access to Employee Self Service
Submit forms to the Benefits Service Centre (BSC) as directed.
BSC Mailing Address
Benefit Service Centre
3980 Quadra Street
Victoria, B.C. V8X 1J9
BSC Fax
604-320-4031
Other questions
Contact MyHR.
This guide describes the benefits program for eligible bargaining unit employees in the BC Public Service. While all efforts have been made to make the guide comprehensive, it doesn't contain all the details in the official documents that legally govern the operation of every benefits plan within the Benefits Program. These plans are subject to change from time to time. In the event of any discrepancy or misunderstanding, benefits will be paid according to the applicable contracts, policies, plan documents, and legislation.
