Appropriate Imaging for Common Situations in Primary and Emergency Care
Effective Date: December 11th, 2019
Recommendations and Topics
- Scope
- Key Recommendations
- Background
- Appropriate Use of CT for Uncomplicated Headache in Adults
- Appropriate Use of CT for Minor Head Injury in Adults and Children
- Appropriate Use of CT for Suspected Pulmonary Embolism in the Non-Pregnant Adult
- Appropriate Imaging for Low Back Pain in Adults
- Appropriate Use of MRI for Hip and Knee Pain in Adults Age ≥ 40
- Resources
Scope
This guideline provides recommendations to primary and emergency care providers on how to assess the need for diagnostic imaging in five common situations: low-back pain (adults), minor head injuries (all ages), uncomplicated headache (adults), hip and knee pain (adults), and suspected pulmonary embolism (non-pregnant adults). Management of these conditions is beyond the scope of this guideline. However, in some cases, notes and alternatives to imaging are provided for additional clinical context.
Key Recommendations
- Imaging is not recommended for uncomplicated headache unless red flags are present.
- CT head scans are not recommended in adults and children who have suffered minor head injuries unless positive for a head injury clinical decision rule.
- Chest CT for suspected pulmonary embolism is not recommended in low-risk patients with a normal D-dimer result.
- Imaging is not recommended for low back pain unless red flags are present.
- MRIs of hip or knee joints are not recommended in patients with co-existent pain and moderate to severe osteoarthritis unless red flags are present.
- Practitioners are encouraged to consult a radiologist if they have any concerns or questions regarding which imaging test is appropriate for a given problem.
The purpose of this guideline is to communicate best practice for imaging in common situations in primary and emergency care, in order to promote appropriate use of imaging resources in BC. Access to diagnostic imaging services, and the ability to respond to emergency/urgent imaging requests, will depend on local availability. When in doubt, direct consultation with a radiologist is encouraged.
Objective: to guide decision-making regarding the use of head CT in adults with uncomplicated headache.
Rationale: CT of the head exposes the patient to radiation. The need for imaging with CT must be balanced against the risk of radiation. When in doubt, consult with the relevant specialist locally or through the RACE Line.
Recommendation: Imaging is not recommended for uncomplicated headache unless red flags are present.
Consider imaging in the following “red flag” situations:2
- sudden onset of severe headache (thunderclap)
- recurrent headache with unexplained focal neurological signs (reference: TOP Alberta)
- new onset in the setting of HIV or cancer
- abnormal neurological exam
- suspected intracranial infection
- new onset or worsening seizure
- new headache age>50
- headache causing awakening from sleep
- papilledema
- focal neurological deficit
- worsening headache frequency or severity in a patient with previous headache history or recent head trauma
- acute head trauma if indicated by CT head clinical decision rule
Think twice before requesting head CT for:
- migraine
- syncope
- temporal arteritis
- multiple sclerosis
- sinusitis
- chronic post-concussion syndrome with normal neurological exam
Key messages for counselling patients if imaging is not indicated:
- Most headaches are benign and self-limiting and do not require a CT head scan or MRI for diagnosis.
Patient and Caregiver Resources
- Imaging Tests for Headaches: When you need them and when you don’t – Choosing Wisely Canada
Appropriate Use of CT for Minor Head Injury in Adults and Children
Objective: to guide decision making regarding the use of head CT in adults and children with minor head injury.
Rationale: CT of the head exposes the patient to radiation. Practitioners should consider the risk of CT radiation exposure. Radiation risks are highest in infants and decrease with age. The following clinical decision rules balance the benefit of identifying a treatable brain injury with the risks associated with radiation exposure. When in doubt, consult with the relevant specialist locally or through the RACE Line.
Recommendation: Do not request CT head scans in patients who have suffered minor head injuries unless positive for a validated head injury clinical decision rule such as:
- Adults age 16+: Canadian CT Head Rule (below)
- Children: PECARN Rule
In situations where CT is not readily available, consultation with a specialist is encouraged to help guide medevac decisions.
Canadian CT Head Rule (for adults and adolescents age 16+)10
The Canadian CT Head Rule can be applied to patients with a “minor” head injury.
In this context, “minor” means a head injury with Glasgow Coma Scale (GCS) 13-15 AND with one of:
- a witnessed loss of consciousness (LOC), or
- amnesia to the head injury event, or
- witnessed disorientation.
A CT head is recommended for patients who fulfil the inclusion criteria above AND any ONE of the following findings:
- High risk (for neurological intervention)
- GCS score <15 at 2h after injury
- Suspected open or depressed skull fracture
- Any sign of basal skull fracture (haemotympanum, ‘raccoon’ eyes, cerebrospinal fluid otorrhoea/rhinorrhoea, Battle’s sign)
- Vomiting ≥2 episodes
- Age ≥65 years
- Medium risk (for brain injury on CT)
- Amnesia > 30 minutes preceding impact
- Dangerous mechanism of injury (e.g. pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall from height >3 feet or five stairs)
Patients who are on blood thinners or have a post-traumatic seizure are excluded from the Canadian CT Head Rule and require individualized assessment.
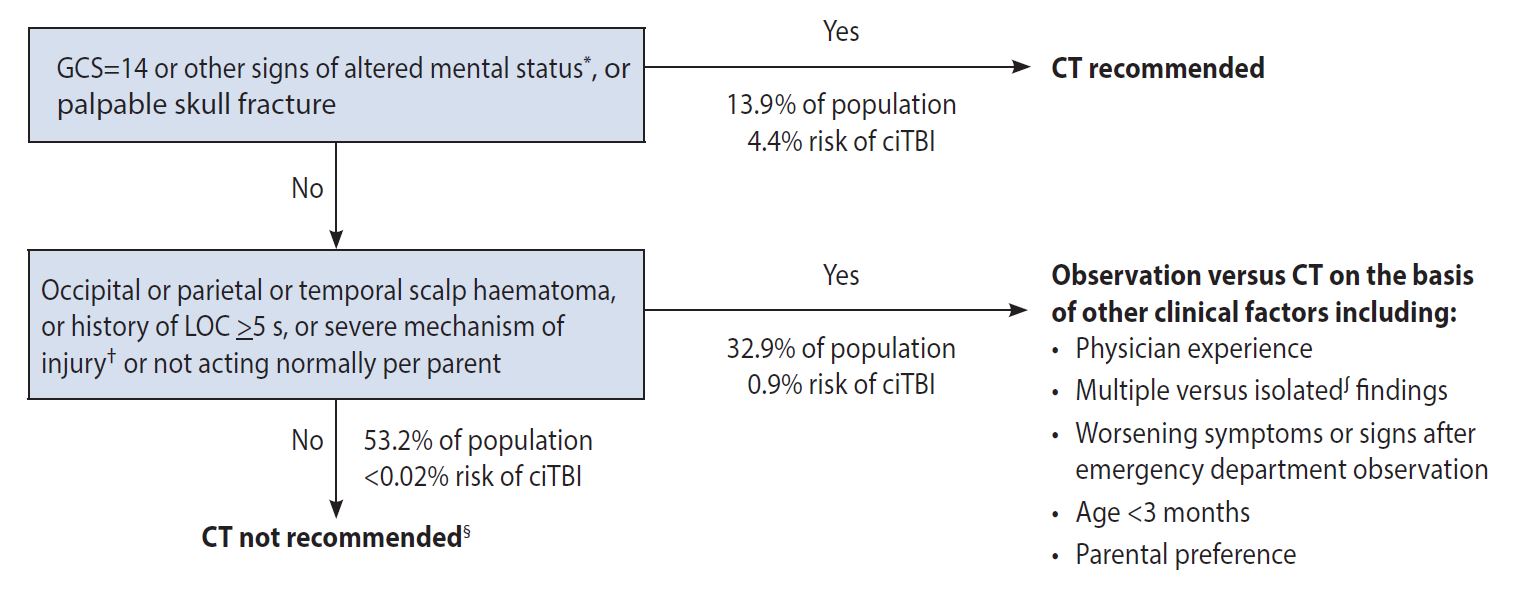
PECARN Rule (for infants and toddlers age < 2 years with GCS score ≥14)11
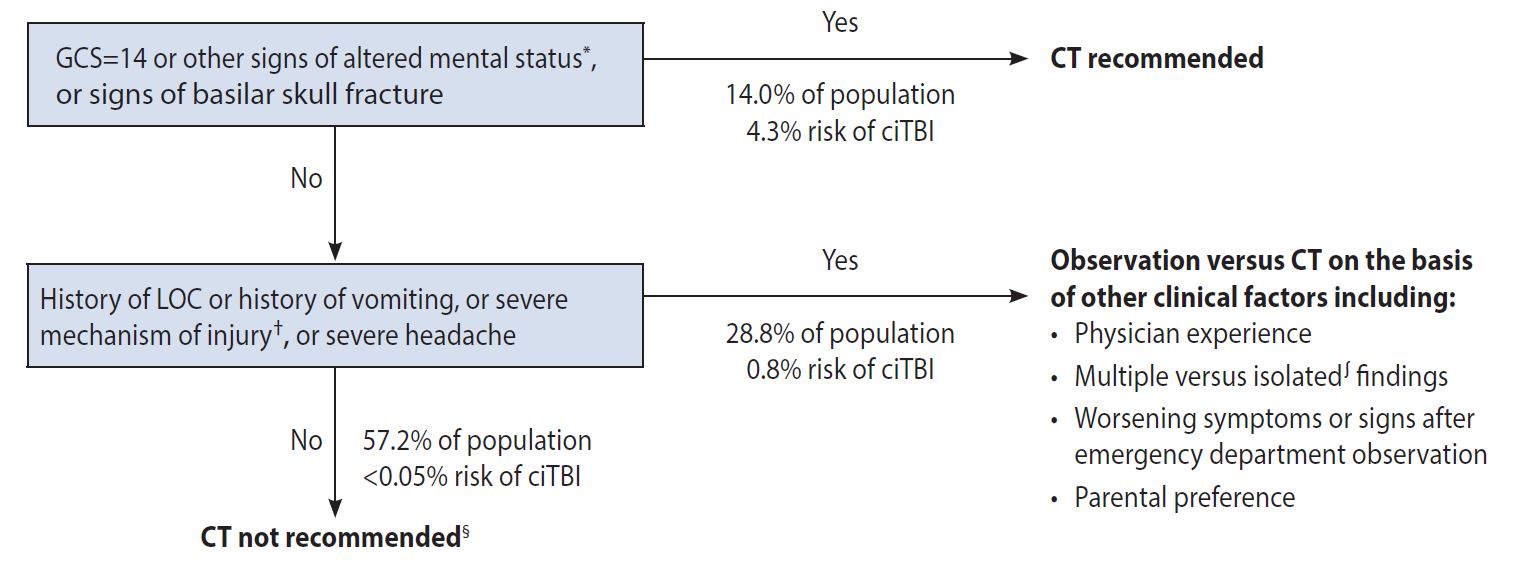
PECARN Rule (for children and toddlers ≥ 2 years with GCS score ≥14)11
 Ɨ Other signs of altered mental status: agitation, somnolence, repetitive questioning, or slow response to verbal communication
Ɨ Other signs of altered mental status: agitation, somnolence, repetitive questioning, or slow response to verbal communication
ƗƗ Severe mechanism of injury: motor vehicle crash with patient ejection, death of another passenger, or rollover; pedestrian or bicyclist without helmet struck by a motorised vehicle; falls of more than 3 feet for children <age 2 or 5 feet for children age 2+, or head struck by a high-impact object
ʃ Patients with certain isolated findings (i.e., with no other findings suggestive of traumatic brain injury), such as isolated LOC, isolated headache, isolated vomiting, and certain types of isolated scalp haematomas in infants older than 3 months, have a risk of clinically-important traumatic brain injury substantially lower than 1%.
¶ Risk of clinically-important traumatic brain injury is exceedingly low, generally lower than risk of CT-induced malignancies. Therefore, CT scans are not indicated for most patients in this group.
Patient and Family Resources:
- BC Children’s Hospital – Head Injury Advice for Parents and Caregivers
- Concussion Awareness Training Tool (for medical professionals, coaches, parents, caregivers, athletes)
 TOP
TOP
Objective: To guide decision making regarding the use of CT in a stable, non-pregnant adult patient presenting with a suspected pulmonary embolism (PE), based on history and physical exam.
Rationale: CT of the chest exposes the patient to radiation. The need for imaging with CT must be balanced against the risk of radiation. When in doubt, consult with the relevant specialist locally or through the RACE Line.
Key points:
- Use a clinical decision rule such as the Wells Score to determine whether the patient is low-risk or high-risk.
- For low risk adult patients:
- If PERC score is 0, then PE is ruled out. There is no need for further investigation.
- If PERC score is >0, a D-dimer should be ordered. If D-dimer is positive, further imaging should be ordered.
- Do not request imaging (CT pulmonary angiogram [CTPA] or ventilation-perfusion [VQ] lung scan) for pulmonary embolism in those with a normal D-dimer result (see below).
- For high risk adult patients: Start empiric treatment with anticoagulant therapy if confirmatory imaging (CTPA, VQ lung scan) is not immediately available.
- High risk PE should be referred to the emergency department and not managed initially in the community.
- Practitioners are reminded to consider risk factors that might alter the pre-test probability. This strategy applies to the majority of people and does not account for unique risk factors (e.g. anabolic steroids, athletes, elderly, paraplegics, etc.). If patients have persistent symptoms beyond 24-48 hours, they should go to the emergency department for further assessment.
Recommendation: When a stable, non-pregnant adult patient presents with signs and symptoms suspicious for PE, the following sequential steps should be done to determine whether a CTPA is required:12
1. Assess pre-test probability using a clinical decision rule (e.g. Wells Score).14,15
- If the total Wells score is ≥ 4.5 (PE likely), proceed to imaging.
- If < 4.5 (PE unlikely), proceed to the pulmonary embolism rule-out criteria (PERC Rule).
|
Variable |
Points |
|---|---|
|
Clinical signs and symptoms of DVT |
3 |
|
No alternative diagnosis more likely than PE |
1.5 |
|
Heart rate >100 bpm |
1.5 |
|
Immobilization ≥3 days or surgery in the past 4 weeks |
1.5 |
|
Previous PE or DVT |
1 |
|
Hemoptysis |
1 |
|
Malignancy |
3 |
2. PERC Rule
- If the patient is low-risk (PE unlikely) and the PERC score is 0 (all of the items are true), the likelihood of PE is <2% and CTPA is not recommended.
- If the patient is low-risk and the PERC score is >0 (one or more items is not true), proceed to D-dimer.
|
Criteria |
Meets criteria |
Does NOT meet criteria |
|---|---|---|
|
Age < 50 |
0 |
1 |
|
Initial heart rate <100 bpm |
0 |
1 |
|
Initial SaO2 > 94% on room air |
0 |
1 |
|
No unilateral leg swelling |
0 |
1 |
|
No hemoptysis |
0 |
1 |
|
No surgery or trauma ≤ 4 weeks |
0 |
1 |
|
No history of VTE |
0 |
1 |
|
No estrogen use |
0 |
1 |
3. D-dimer: CTPA is not recommended if D-dimer is below the normal range for your institution.
Clinicians may use a negative age-adjusted D-dimer result using a high-sensitivity assay to exclude the diagnosis of PE in patients older than 50 years who have a low risk for acute PE according to a validated risk score (e.g. Wells score or simplified, revised Geneva score).
For more detailed guidance on diagnosis of PE, refer to the BC Emergency Medicine Network Point-of-Care Emergency Clinical Summary, available from: bcemergencynetwork.ca/clinical_resource/pulmonary-embolism-diagnosis/
|
Diagnostic imaging for suspected PE in pregnant patients
|
|---|
 TOP
TOP
Appropriate Imaging for Low Back Pain in Adults
Objective: to guide decision making regarding whether imaging is needed in an adult patient presenting to primary care or the emergency department with acute low back pain (defined as low back pain of less than 6 weeks duration).
Rationale: X-ray and CT expose the patient to radiation. The need for imaging must be balanced against the risk of radiation. When in doubt, consult with the relevant specialist locally or through the RACE Line. Imaging of low back pain without red flags is unlikely to change management or improve treatment.3–7 Acute (new onset) low back pain usually resolves by 6 weeks.6,8
Recommendation: Diagnostic imaging (x-ray, CT or MRI) for low back pain of less than 6 weeks duration is not recommended unless one of the following red flags is present:2,9
- severe or progressive neurologic deficit
- significant acute traumatic event immediately preceding onset of symptoms
- suspected compression fracture (risk factors include long term steroid use)
- suspected cancer, cancer related complication, or history of cancer
- suspected infection (e.g. discitis/osteomyelitis, epidural abscess; risk factors include history of IV drug use)
- suspected spinal epidural hematoma
- cauda equina syndrome
- older age with first episode of severe back pain
Key messages for counselling patients if imaging is not indicated:
- Acute (new onset) low back pain usually resolves within 6 weeks
- CT, MRI and X-rays for uncomplicated low back pain do not help patients get better faster and may expose them to unnecessary risks and incidental findings. There is often poor correlation between imaging findings and symptoms.
- Low back pain is very common and often caused by back strain. It usually resolves within weeks without medical treatment. Check back with your health care provider if the pain is getting worse not better, or if you have new symptoms.
- Treat low back pain with heat, acetaminophen, NSAIDS, and gradual return to usual activities.
- Exercise may decrease low back pain symptoms5 and may reduce recurrence6
- Address fear of activity and return to work and normal activities7
- Recommend physiotherapy if exercise persistently makes the pain worse6
Practitioner resources
- BC Guideline Managing Pain: link to be added when it is available.
- BC Emergency Medicine Network: Clinical Resource - Low Back Pain
Patient and caregiver resources
- Patients can call 8-1-1 to speak with an exercise physiologist to receive individualized care including:
- exercises to address low back pain
- advice on how to increase physical activity
- support for motivation, education, identifying and overcoming barriers, and return to work
- Choosing Wisely Patient Handout - Imaging Tests for Lower Back Pain: When you need them and when you don’t (available in French, Arabic, Punjabi, Simplified Chinese, Spanish, and Tagalog)
- HealthLinkBC: Low Back Pain: Exercises to Reduce Pain
 TOP
TOP
Appropriate Use of MRI for Hip and Knee Pain in Adults Age ≥ 40
Objective: to guide decision-making regarding whether MRI is needed in a patient ≥ age 40 presenting to primary care or the emergency department with hip or knee pain and osteoarthritis in the subject joint.
Rationale: The purpose of an MRI for knee or hip is primarily for surgical planning. In most cases, using MRI does not add useful information for patients with moderate-to-severe osteoarthritis (OA) especially for those with chronic degenerative conditions. A weight-bearing x-ray is recommended to identify OA.
Recommendation: In the absence of red flags, acute or chronic hip or knee pain with plain film x-ray evidence of moderate to severe osteoarthritis (OA) does not require MRI. MRI should be reserved for evaluation of possible red flag diagnoses or common conditions treatable with arthroscopy, e.g. meniscus and ligamentous tears.
MRI Knee and Hip Appropriateness Criteria
For patients 40 years of age and older, one of the following red flags must apply in order to be eligible for MRI knee or hip:
- MRI was recommended on a previous imaging report (please attach report)
- Previous knee or hip surgery*
- Suspected infection*
- Suspected tumour
- Osteonecrosis
- Fixed locked knee*
- Patient had a weight-bearing x-ray within the past 6 months and referring clinician has confirmed mild or no evidence of osteoarthritis in the knee or hip
*Knee or hip pain in the settings of previous surgery, suspected infection, or fixed locked knee may be urgent or emergent. Consider discussion with an orthopedic surgeon prior to requesting an MRI. All orthopedic emergencies require immediate consultation.
Key messages for counselling patients:
- Having an x-ray can inform the appropriate investigation pathway
- In absence of red flag symptoms, there is no evidence for the utility of MRI in patients with significant OA.
- Most orthopaedic surgeons do not require obligatory MRI prior to consultation. If an MRI is required, the surgeon can request it.
- Discuss options for treatment and pain management including a trial of acetaminophen and NSAIDS.
Patient and caregiver resources:
MRI for Knee and Hip – when is it appropriate? Information for patients (Vancouver Coastal Health)
 TOP
TOP
Resources
Practitioner Resources
- RACE Line: raceconnect.ca
- A telephone consultation line for select specialty services for physicians, nurse practitioners and medical residents. If the relevant specialty area is available through your local RACE line, please contact them first. Contact your local RACE line for the list of available specialty areas. If your local RACE line does not cover the relevant specialty service or there is no local RACE line in your area, or to access Provincial Services, please contact the Vancouver Coastal Health Region/Providence Health Care RACE line.
- Vancouver Coastal Health Region/Providence Health Care: www.raceconnect.ca or 604-696-2131 or 1-877-696-2131
- Northern RACE: 1-877-605-7223 (toll free)
- Kootenay Boundary RACE: www.divisionsbc.ca/kootenay-boundary/our-impact/team-based-care/race-line 1-844-365-7223 (toll free)
- Fraser Valley RACE: www.raceapp.ca
- South Island RACE: www.raceapp.ca/ or see www.divisionsbc.ca/south-island/race
- Pathways: pathwaysbc.ca
- An online resource that allows GPs and nurse practitioners and their office staff to quickly access current and accurate referral information and wait times for specialists and specialty clinics. Pathways also has hundreds of patient and physician resources that are categorized and searchable.
- An online resource that allows GPs and nurse practitioners and their office staff to quickly access current and accurate referral information and wait times for specialists and specialty clinics. Pathways also has hundreds of patient and physician resources that are categorized and searchable.
- BC Emergency Medicine Network: https://emergencycarebc.ca/
- Includes practitioner resources, point-of-care clinical summaries, and patient handouts.
- Includes practitioner resources, point-of-care clinical summaries, and patient handouts.
- Lower Mainland Medical Imaging MRI Central Intake Program: http://www.phsa.ca/our-services/programs-services/lower-mainland-medical-imaging
 TOP
TOP
Associated Documents
- List of Contributors (PDF, 166KB)
- BC Guideline: Ultrasound Prioritization
- BC Guideline: Ankle Injury – X-Ray for Acute Injury of the Ankle or Mid-Foot
How this Guideline was Developed
The five recommendations in this guideline were agreed to by a provincial expert advisory group on medical imaging in British Columbia.1 The recommendations were developed by consensus to decrease the rate of inappropriate medical imaging.1 They are informed by the Canadian Association of Radiologists (CAR) Choosing Wisely Canada Top 5 recommendations.2
Where available, key references are provided. In situations where there is a lack of rigorous evidence, we provide best clinical opinion to support decision making and high-quality patient care.
References
- Forster B, Chan V, Coleman J, Houston D, Quality, Performance, Service Distribution Working Group. When to image (and when not to image). A toolkit for ensuring appropriate use of medical imaging. Unpublished; 2017.
- Canadian Association of Radiologists. Five things physicians and patients should question in radiology. [Internet]. Choosing Wisely Canada. [cited 2019 May 3]. Available from: https://choosingwiselycanada.org/radiology/
- Chou R, Fu R, Carrino JA, Deyo RA. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet Lond Engl. 2009 Feb 7;373(9662):463–72.
- Chou R, Qaseem A, Owens DK, Shekelle P, Clinical Guidelines Committee of the American College of Physicians. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011 Feb 1;154(3):181–9.
- National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management NICE guideline [NG59] [Internet]. NICE; 2016 [cited 2019 Apr 23]. Available from: https://www.nice.org.uk/guidance/ng59
- Institute of Health Economics Alberta. Evidence-Informed Primary Care Management of Low Back Pain Clinical Practice Guideline [Internet]. Toward Optimized Practice (TOP); 2015 [cited 2019 Apr 23]. Available from: http://www.topalbertadoctors.org/download/1885/LBPguideline.pdf?_20190423201424
- Thorson D, Campbell R, Massey M, Mueller B, McCathie B, Richards H, et al. Health Care Guideline: Adult Acute and Subacute Low Back Pain [Internet]. Institute for Clinical Systems Improvement; 2018 [cited 2019 May 3]. Available from: https://www.icsi.org/wp-content/uploads/2019/01/March-2018-LBP-Interactive.pdf
- Chiodo A, Alvarez D, Graziano G, Haig A, Van Harrison R, Park P, et al. Michigan Medicine Quality Department Clinical Care Guidelines: Acute Low Back Pain [Internet]. University of Michigan; 2010 [cited 2019 May 3]. Available from: http://www.med.umich.edu/1info/FHP/practiceguides/back/back.pdf
- Min A, Chan VWY, Aristizabal R, Peramaki ER, Agulnik DB, Strydom N, et al. Clinical Decision Support Decreases Volume of Imaging for Low Back Pain in an Urban Emergency Department. J Am Coll Radiol JACR. 2017 Jul;14(7):889–99.
- Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head Rule for patients with minor head injury. The Lancet. 2001 May 5;357(9266):1391–6.
- Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. The Lancet. 2009 Oct;374(9696):1160–70.
- Kline JA, Kabrhel C. Emergency Evaluation for Pulmonary Embolism, Part 2: Diagnostic Approach. J Emerg Med. 2015 Jul;49(1):104–17.
This guideline is based on expert BC clinical practice current as of the Effective Date. This guideline was developed by the Guidelines and Protocols Advisory Committee and approved by the Medical Services Commission.
|
The principles of the Guidelines and Protocols Advisory Committee are to:
|
Disclaimer The Clinical Practice Guidelines (the "Guidelines") have been developed by the Guidelines and Protocols Advisory Committee on behalf of the Medical Services Commission. The Guidelines are intended to give an understanding of a clinical problem and outline one or more preferred approaches to the investigation and management of the problem. The Guidelines are not intended as a substitute for the advice or professional judgment of a health care professional, nor are they intended to be the only approach to the management of clinical problems. We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. If you need medical advice, please contact a health care professional.

