Extended Learning Document: Primary Care Approaches to Addressing the Impacts of Trauma and Adverse Childhood Experiences (ACEs)
Effective Date: January 17, 2024
Recommendations and Topics
Purpose
All individuals experience trauma throughout their lives.1 These traumatic experiences may be previous events, or they may be current. The health care community’s understanding of trauma’s impacts on our health continues to evolve, particularly in the context of the In Plain Sight Report highlighting the experiences of Indigenous peoples in Canada, the ongoing toxic drug crisis, and mass traumatic events, such as natural disasters, warfare and genocide.2,3 Primary care providers are encouraged to learn how trauma affects an individual's and community’s health, as well as their utilization of the health care services, and health care experiences.
This extended learning document seeks to introduce primary care providers to the concept of trauma-informed practice (TIP). It provides information about tools including, but not limited to, the Adverse Childhood Experiences (ACEs) questionnaire. This document also provides additional resources for ongoing learning and professional/ personal development.
This is not a clinical practice guideline as research in this area is still evolving, especially the evidence for the use of the ACEs questionnaire in clinical practice. The focus of the document is on adults. While some resources are referenced for the pediatric population, history taking and management of adverse childhood experiences in children and adolescents are outside the scope of this guideline.
Key Learnings
- Build a strong, ongoing, consistent, and trusting relationship with patients. This is important to successfully address difficult topics in a culturally safe way and to support an individual’s ability to make positive changes over time. This enables primary care practitioners providing longitudinal care to better support their patients to improve their well-being, address past experiences, and give hope.1 While an ongoing relationship is important, there will be episodic encounters where practicing in a trauma-informed way will be imperative, to ensure patients return to seek care (e.g., walk-in or emergency department setting).
- Recognize and respect the prevalence of historical, intergenerational and current trauma, as well as the many ways that trauma can be experienced. See Indian Hospitals in Canada to learn more.
- Be sensitive to trauma-informed principles in patient interactions.
- Practice a reflective, continuous commitment to ongoing education, which is an important aspect of trauma-informed practice (TIP).
- Practice trauma-informed care, including considerations for staff and clinicians who have experienced trauma in their own lives.1,4 This trauma may come from personal experiences, or it could be secondary trauma experienced during exposure to another individual's traumatic experiences.
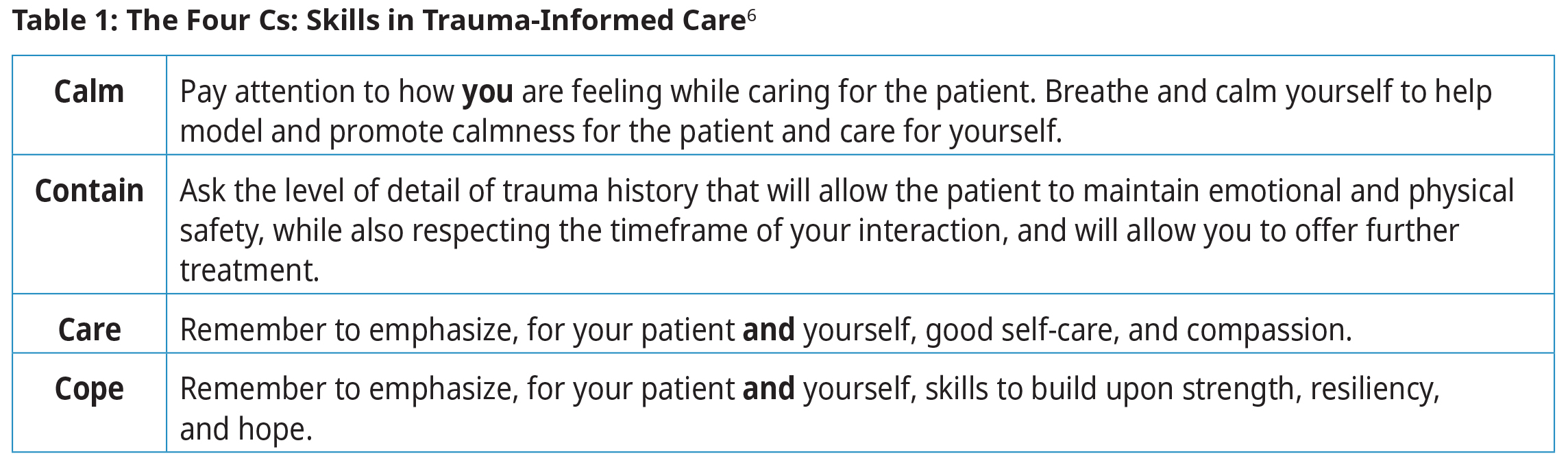
- It is important that healthcare providers build an informal system of peer support that they can draw on or contribute to.1,5 Skills, such as “The Four Cs,” can support care providers’ well-being while delivering TIP (see Table 1 below).6 The Physician Health Program (PHP) offers a confidential 24-hour intake and crisis support line (1-800-663-6729).
-
It is not enough to have cultural awareness and cultural sensitivity to improve access and quality of health care services. It is imperative that all these concepts are applied in practice as practitioners continue their cultural safety and humility journey and learning (see Figure 1 below).
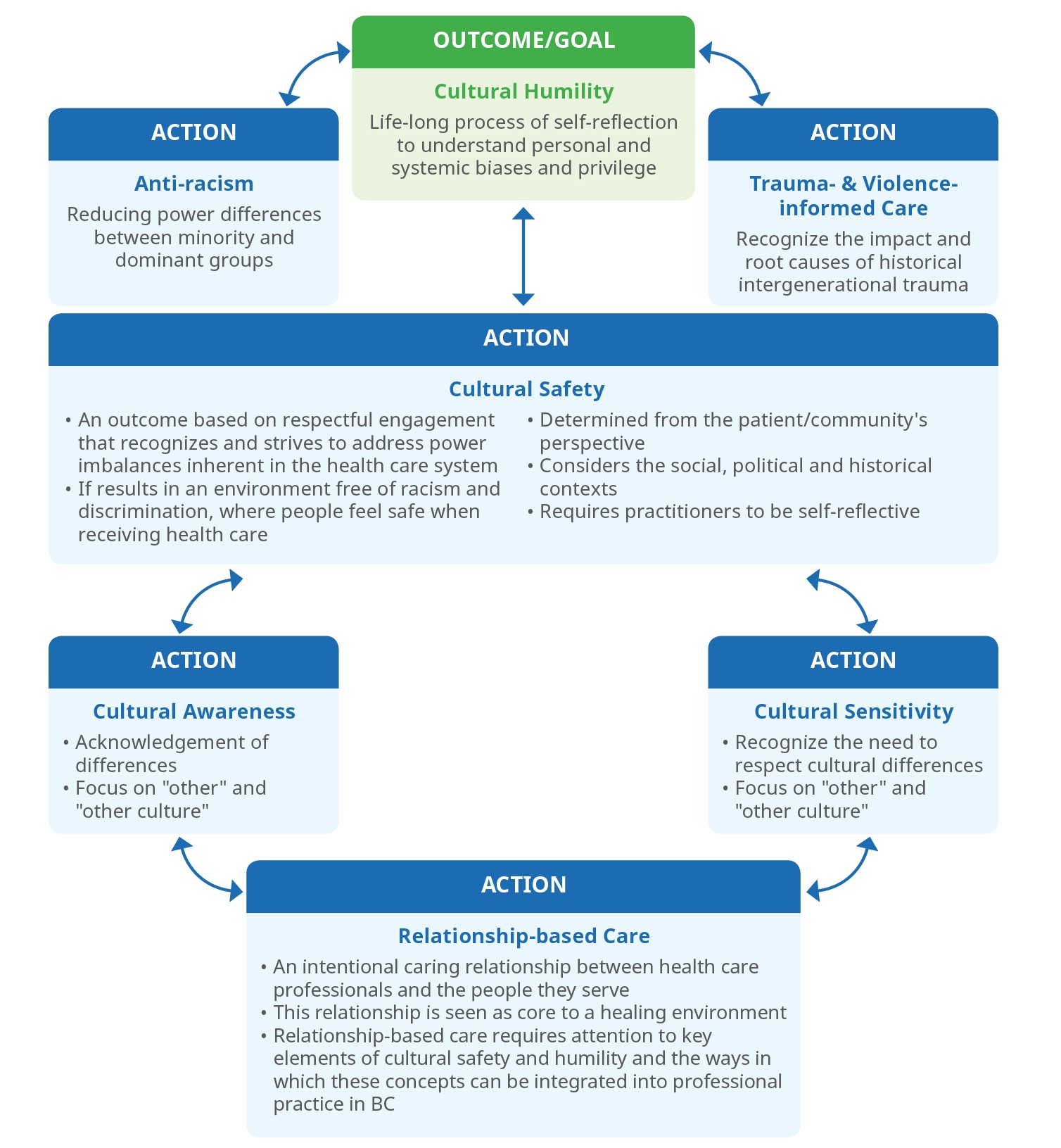
*Adapted from FNHA's booklet Creating a Climate for Change and the PHCA's document Common Definitions on Cultural Safety: Chief Public Health Officer Health Professional Forum. See Appendix A: Definitions for more information.
Background
Trauma and its sources
Traumatic experiences may be experienced individually or collectively. Although trauma spans across all races, ages, and socioeconomic statuses, some populations are exposed to trauma at higher rates and with greater frequency than others, e.g., minorities and patients who experience or who have familial experience with chronic economic stress and poverty, incarceration, homelessness, and substance use.1 Additionally, Indigenous communities continue to bear the health impacts of multigenerational and historical trauma because of the ongoing effects of colonization, e.g., higher rates of diabetes, heart disease, and HIV/AIDS.1,2,7–9
Indigenous Patients and TIP in British Columbia (BC)
Assigned trauma scores (e.g., ACEs) may be reminiscent of other harmful colonial practices and may not feel safe to all Indigenous patients. Consider using a tool developed by Indigenous peoples, for Indigenous peoples, or referring to an Indigenous provider or service if you are unsure of your own ability to provide culturally safe care. Please see Appendix H: Patient, Family, and Caregiver Resources for a list of Indigenous-centered resources.
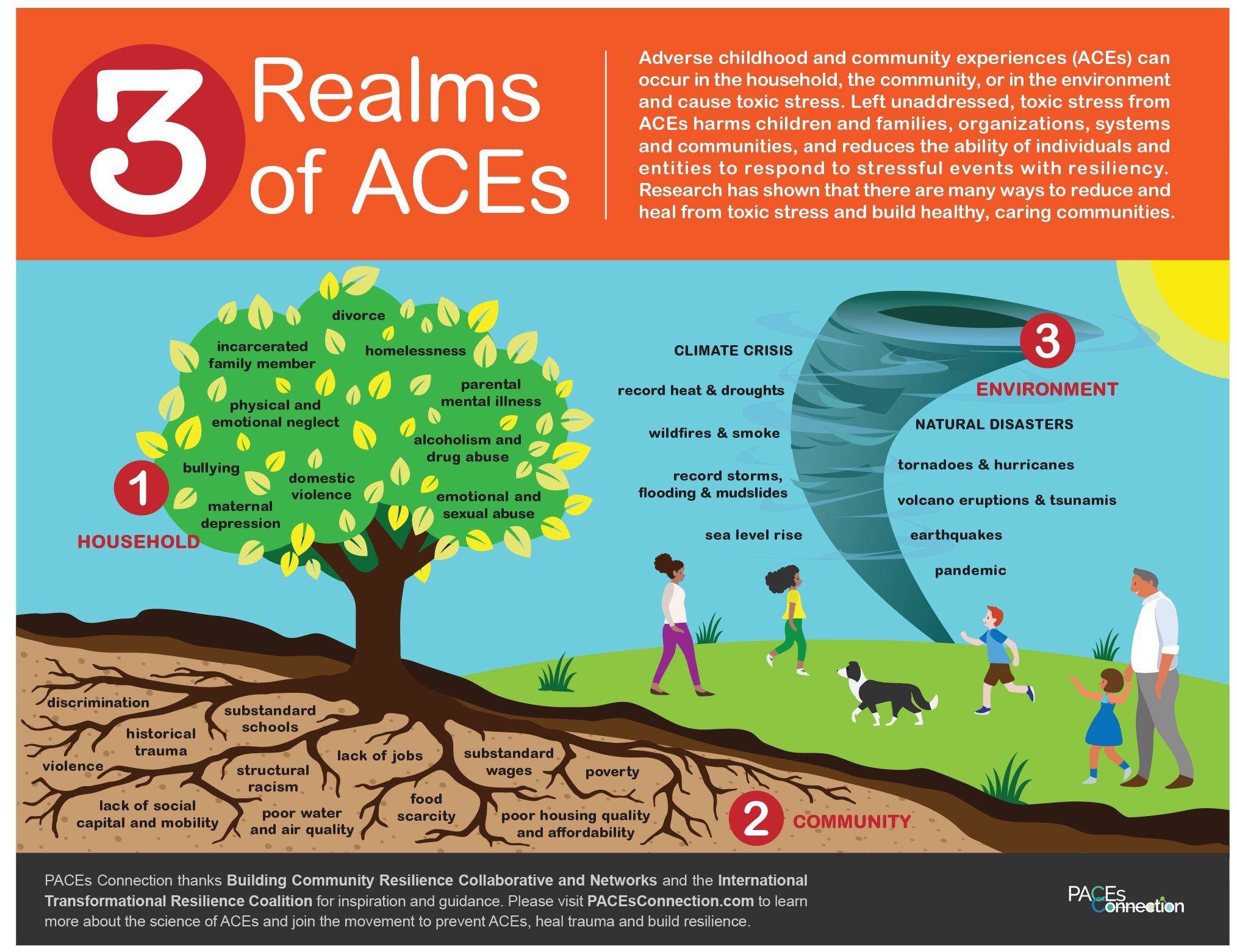
As illustrated in Figure 2: 3 Realms of ACEs10 below, the community environment can have a direct impact on an individual’s exposure to trauma. Traumatic experiences in childhood are risk factors for many leading causes of disease, death, disability, poor health, and other social challenges in adults.11 For more information on how trauma can contribute to health outcomes, please see Appendix E: Developmental Impact of Adverse Childhood Experiences (ACEs).
Figure 2: 3 Realms of ACEs12
Trauma-informed practice (TIP)
Trauma-informed approaches are based on resilience, a consistent relationship of trust between patient and provider, and creation of a consistent environment where the patient feels connected, safe, respected, and able to rebuild a sense of control and empowerment.
TIP benefits all patients regardless of their trauma history and should be offered to everyone as a universal precaution. Without this approach during healthcare visits, patients may be retraumatized.
Refer to Practitioner Resources and Appendix F: Avoiding Practice Traps for further support.
ACEs and its relevance to TIP
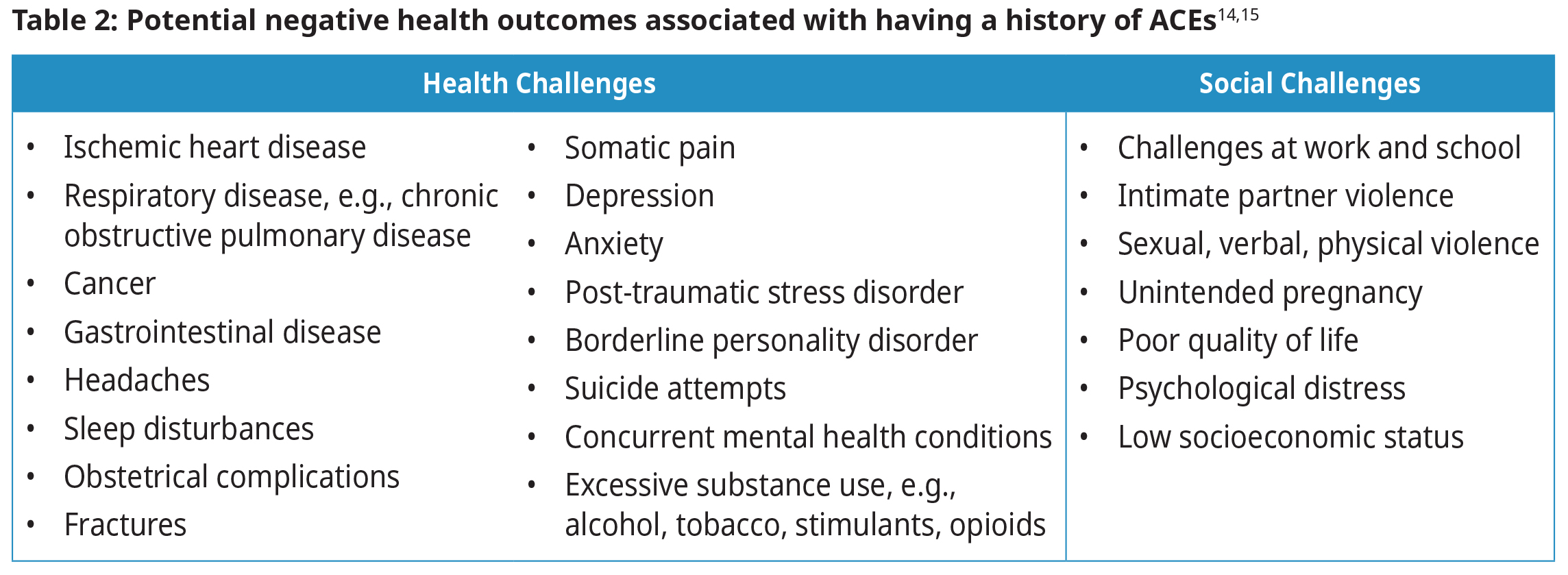
Childhood experience of trauma can affect the developing brain and body, resulting in neurobehavioral, social, emotional, and cognitive changes, all of which can have a lifelong impact on the patient’s health.1,11,14
Structural and neurophysiological changes occur when the developing brain experiences chronic and pervasive stress over time, impacting cortisol regulation. Individuals who have been exposed to trauma may experience a wide range of mental health conditions including anxiety, depression, posttraumatic stress disorder, and suicide attempts.1,11,14 Refer to Appendix E: Developmental Impact of Adverse Childhood Experiences (ACEs) for more information.
Figure 3: The conceptual framework for the ACE Study. ACEs may influence health and well-being throughout a patient's lifespan.13
Patients who have experienced ACEs may self-medicate using alcohol and other substances, or engage in risky behaviors, such as self-harm, to cope.15 Alcohol use disorder (AUD) is a chronic relapsing and remitting medical condition. Regardless of adverse social, occupational, or health repercussions, individuals are unable to stop or control their alcohol use. Any coping mechanisms should be addressed respectfully and without judgement.13 Be aware of supports for patients with substance use, as described in safer drinking guidelines. There are alarming health disparities that exist between Indigenous and non-Indigenous populations, due to the ongoing effects of oppression and colonization.8
The ACEs Questionnaire
The ACEs questionnaire is composed of ten questions and invites reflection upon specific experiences of developmental trauma. For detailed information on how to appropriately use the ACEs questionnaire in the primary care setting, please see Appendix C: Adverse Childhood Experiences [ACEs] Questionnaire and Appendix D: Considerations for ACE Questionnaire Use in the Primary Care Setting. As ACEs is an evolving field of study, providers who might perform the ACEs questionnaire are encouraged to engage in continuing education. Please see Practitioner Resources for more information. 11
The ACEs questionnaire can be a useful tool under the right circumstances for some patients, but it is not a one-size-fits-all solution. While some patients may feel validated by a quantitative score, others may feel devalued and re-traumatized (or “triggered”) by such an assessment. It is important to be aware that the numerical score indicates relative risk, not an absolute outcome (positive or negative). The impact of traumatic experiences on a patient’s health depends on the supports available to them since the time of the event(s).1,13 A low or zero score does not denote the absence of trauma. Refer to Appendix D: Considerations for ACE Questionnaire Use in the Primary Care Setting.
The Deveraux Adult Resilience Survey (DARS)
The DARS is a 23-item, strengths-based reflective checklist that provides adults with information about their resilience, relationships, and skills.16 The DARS is supplemented by examples, reflection and an action plan that can be used to help individuals build on their existing strengths. A copy of the DARS is available in Appendix B: Devereaux Adult Resilience Survey (DARS) and Adverse Childhood Experiences (ACEs) Questionnaire.
Trauma and attitudes towards medical care
In addition to physical and mental health, a history of trauma can have a profound effect on a patient’s attitudes toward medical care.1 Trauma-induced feelings of guilt, shame, rage, isolation, or powerlessness can be exacerbated by the power dynamic experienced in the provider-patient relationship.6 Patients may experience anxiety due to examinations, procedures, or healthcare settings which remind them of their traumatic experience(s). Previously, patients may have had encounters with providers who were unaware of or unfamiliar with trauma-informed practices, and unintentionally retraumatized them. This combination of experience, emotion, and relationships may explain why survivors are more likely to default to acute and emergency care than preventive care. Also refer to Indian Hospitals in Canada to learn more.
Benefits of addressing trauma in primary care
Addressing sources of mental and physical stress is important in preventing negative patient health outcomes. Acknowledging trauma in the primary care setting can:
- Provide a supportive, healing and consistent relationship for safe attachment, especially for those who have not had that experience.
- Reduce stigma by demonstrating that the practice is a safe and non-judgmental environment.
- Encourage patients to become proactive partners in their healing journey by validating their strengths.
A patient is more likely to share and want to work on a health condition when they feel safe with their care provider.1
Assessment for trauma
The best way to assess trauma is to approach each patient’s case with respect and consideration. Give some thought as to how and when to conduct the assessment, whether evaluating will be for current or past trauma(s), and if assessment instruments will be delivered in person, or completed virtually.1 Regardless of how assessment is undertaken, respect should be shown when survivors of trauma do not wish or are unable to discuss their experiences.
A trusting, consistent relationship is essential and takes time to develop. This is an important aspect prior to conducting a trauma evaluation.1,6 Even with a trusting, consistent relationship in place, patients may change their minds about disclosing traumatic experiences after initially expressing interest. Trauma is most felt when an individual feels alone and unsafe in a chaotic environment. The support for the individual is that they need to feel that they are seen, heard, held and valued in the encounter(s). Remain patient, avoid stigmatizing survivors, and focus on resilience rather than pathology.13 Practitioners need to know how to identify their own triggers and be mindful of self-care. This allows the practitioner to approach the individual in a caring way to de-escalate triggering situations and support patients as needed. Consider asking the question, 'What happened to you?' rather than 'What's wrong with you?' when addressing problems that may be related to past trauma.
Supporting patients who have experienced trauma
Asking, listening, and validating is itself an intervention that can support patient health outcomes, and promote healing and recovery.4,17 Whenever possible, providers should identify patients’ strengths and build on them.13 Consider offering a resilience questionnaire e.g., Appendix B: Devereaux Adult Resilience Survey (DARS) and/or building a resource list (see Appendix H: Patient, Family, and Caregiver Resources).
Another supportive technique to consider is motivational interviewing. Motivational interviewing techniques assist patients in making changes that improve their own personal sense of well-being (refer to Appendix G: Validating and Invalidating Statements and Curious Questions). For more information on motivational interviewing, please refer to Adult Mental Health Cognitive Behavioural Interpersonal Skills Tools for strategies and techniques.
Examples of open ended, resilience-oriented questions.
"What are you already doing to look after yourself [your family, children, etc.]?"
"How have you managed to get through the tough times in your life?"
"What are your hopes for the future?"
Source: BC TIP Guide
Refer to the continued learning section for motivational learning resources.
Recognizing re-traumatization and secondary trauma
Re-traumatization is a “conscious or unconscious reminder of past trauma that results in a re-experiencing of the initial event”.1 A wide variety of experiences during a clinical encounter could be re-traumatizing. These experiences include but are not limited to personal questions that may be distressing or result in a sense of loss of or lack of privacy, physical touch, or the power differential in the patient–physician relationship.
The Physician Health Program (PHP) offers a confidential 24-hour intake and a crisis support line 1-800-663-6729. Additional resources for provider wellness can be found on the Resources on Vicarious Trauma website. A fact sheet specific to the experience of vicarious trauma in Indigenous communities developed by the Thunderbird Partnership Foundation can be found here.
Resources
Appendices
- Appendix A: Definitions
- Appendix B: Devereaux Adult Resilience Survey (DARS)
- Appendix C: Adverse Childhood Experiences (ACEs) Questionnaire
- Appendix D: Considerations for ACE Questionnaire Use in the Primary Care Setting
- Appendix E: Developmental Impact of Adverse Childhood Experiences (ACEs)
- Appendix F: Avoiding Practice Traps
- Appendix G: Validating and Invalidating Statements and Curious Questions
- Appendix H: Patient, Family, and Caregiver Resources
Associated Documents
Practitioner Resources
Trauma-Informed Practice
- UBC CPD IPL Group Trauma Informed Practice: Whu’nus’en – We See in Two Worlds: Trauma Sensitive Practices for Collectively Healing in Relationship found on https://ubccpd.ca/
- BC Trauma-Informed Practice Guide: https://cewh.ca/wp-content/uploads/2012/05/2013_TIP-Guide.pdf
- Cognitive Behavioural Interpersonal Skills (CBIS) - Indigenous: pspexchangebc.ca/course/view.php?id=70§ion=4
- EQUIP Trauma and Violence Informed Care Resources: https://equiphealthcare.ca/tvic-workshop/
- The Trauma-Informed Toolkit – Klinic Community Health Centre: gbsurvivors.org/wp-content/uploads/2017/05/Trauma-Toolkit.pdf
- Handbook on Sensitive Practice for Health Care Practitioners - Lessons from adult survivors of childhood sexual abuse: publications.gc.ca/collections/collection_2010/aspc-phac/HP20-11-2009-eng.pdf
- Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Improvement Protocol - Trauma-Informed Care in Behavioral Health Services: https://store.samhsa.gov/product/tip-57-trauma-informed-care-behavioral-health-services/sma14-4816
- Complex Trauma Resources for Clinicians: https://www.complextrauma.ca/resources
- Resources on Vicarious Trauma: https://www2.gov.bc.ca/assets/gov/health/managing-your-health/mental-health-substance-use/child-teen-mental-health/vicarious_trauma_and_organization_resource_list.pdf
- The Physician Health Program (PHP): Offers a confidential 24-hour intake and a crisis support line 1-800-663-6729.
Indigenous Cultural Safety (ICS)
- San’yas Indigenous Cultural Safety Training - Provincial Health Services Authority: sanyas.ca
- ICS Hummingbird Level 1 – Foundations – Available in some regional health authorities and found on https://medicalstaff.vch.ca/.
- Resources and Webinars about Cultural Safety and Humility - First Nations Health Authority: https://www.fnha.ca/what-we-do/cultural-safety-and-humility
- Anti-Racism, Cultural Safety & Humility Framework - First Nations Health Authority: https://www.fnha.ca/Documents/FNHA-FNHC-FNHDA-Anti-Racism-Cultural-Safety-and-Humility-Framework.pdf
- British Columbia Cultural Safety and Humility Standard – https://healthstandards.org/standard/cultural-safety-and-humility-standard/
- For the Next Seven Generations – for the Children – Island Health’s Indigenous Health Program: https://www.islandhealth.ca/learn-about-health/indigenous-health/indigenous-health-cultural-safety
- Cultural safety modules – through Continuing Studies at the University of Victoria:
- Peoples’ Experiences of Colonization
- Peoples’ Experiences of Oppression
- Peoples’ Experiences of Colonization in Relation to Health Care
- Practicing Cultural Safety and Humility in the Response to COVID-19 - BC College of Family Physicians: https://bccfp.bc.ca/wp-content/uploads/2020/05/Practising-cultural-safety-and-humility-in-response-to-COVID-19.pdf
- R.E.S.P.E.C.T. Model of Cross-Cultural Communication: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2847117/?tool=pubmed
- In Plain Sight – Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care: https://engage.gov.bc.ca/addressingracism/
- Other health authority cultural health and wellness resources:
- Northern Health: Local Cultural Resources
- Vancouver Coastal Health: Indigenous Cultural Safety Policy
- Fraser Health: Cultural Safety and Humility
- Interior Health: “Cultural Safety in Practice – How to be an Ally” (video)
- Island Health: Cultural Safety
- Primary Care Networks: Indigenous Engagement and Cultural Safety Guidebook
- Anti-Racism – BC College of Family Physicians: https://bccfp.bc.ca/anti-racism-2/
- Health Quality BC: Culturally Safe Engagement: What Matters to Indigenous (First Nations, Métis & Inuit) Patient Partners?
- BC Public Service: Cultural Agility
- Rise Above Racism: Anti-Indigenous Racism Resources
Refugees
- BC Refugee Hub: Mental Health Toolkit for Refugees and Refugee Claimants – BC Refugee Hub
- Vancouver Association for the Survivors of Torture (VAST): VAST is BC's largest centre for refugee and newcomer mental health and supports individuals who arrive in BC with psychological trauma and vulnerable status. VAST BC
- Vancouver Island Counselling Centre for Immigrants and Refugees (VICCIR): VICCIR
2SLGBTQIA+
- QMUNITY: BC’s queer resource centre. www.qmunity.ca or 604-684-5307
- TransCare BC: http://www.phsa.ca/transcarebc/
- Trans Lifeline: A trans-led organization that connects trans people to the community, support, and resources. Telephone number: 1 (877) 330-6366
- Victoria Pride Society: Victoria 2SLGBTQIA+ youth resources
Continuing Professional Development
- Practice Support Program ACEs module: for small group learning and individual support
- Alberta Family Wellness Initiative - The Brain Story Certification: https://www.albertafamilywellness.org/training
- Positive and Adverse Childhood Experiences (PACEs) Connection: https://www.pacesconnection.com/
- Workshops and Information on Trauma and Dissociation for physicians and nurses: https://www.beyond-the-cycle-of-trauma.org/
- VEGA (Violence, Evidence, Guidance and Action) Project: evidence-based guidance and education resources including care pathways, scripts, and how-to videos for responding to child maltreatment, intimate partner violence, and children’s exposure to intimate partner violence: https://vegaproject.mcmaster.ca/
- Motivational Interviewing:
- UBC CPD: Motivational Interviewing eLearning
- The Centre for Collaboration, Motivation and Innovation: Motivational Interviewing
- Motivational Interviewing Network of Trainers (MINT)
- Change Talk Associates
- The Centre for Addiction and Mental Health
- PsyMontreal
Pediatrics
- Collaborative Toolbox: a ‘one-stop-shop’ of resources created and curated by members of the BC Child and Youth Mental Health and Substance Use Collaborative: http://www.collaborativetoolbox.ca/
- Canadian Pediatric Society Position Statement – Relationships Matter: How clinicians can support positive parenting in the early years: https://www.cps.ca/en/documents/position/positive-parenting
- Stress Health: practical resources for parents to build resilience: stresshealth.org/
- Complex Trauma: Facts for Caregivers. A pdf guide for foster parents.
- Perinatal Services BC: ‘Honouring Indigenous Women’s and Families’ Pregnancy Journeys: A Practice Resource to Support Improved Perinatal Care Created by Aunties, Mothers, Grandmothers, Sisters, and Daughters’
Rapid Consultation Services
- RACE: Rapid Access to Consultative Expertise Program – www.raceconnect.ca A phone consultation line for physicians, nurse practitioners and medical residents.
If relevant specialty area is available through your local RACE line, please contact them first.
Contact your local RACE line for the list of available specialty areas. If your local RACE line does not cover the relevant specialty service or there is no local RACE line in your area, or to access Provincial Services, please contact the Vancouver/Providence RACE line.
- Vancouver Coastal Health Region/Providence Health Care: www.raceconnect.ca www.raceapp.ca (tip: download the RACEapp+ to your device from the Apple or Android stores)
- 604-696-2131 (Vancouver) or 1-877-696-2131 (toll free) Available Monday to Friday, 8 am to 5 pm, excluding statutory holidays.
- Northern RACE
- 1-877-605-7223 (toll free)
- Kootenay Boundary RACE
- 1-844-365-7223 (toll free)
- Fraser Valley RACE: www.raceapp.ca (tip: download the RACEapp+ to your device from the Apple or Android stores)
- Vancouver Island RACE: to register, please visit www.raceapp.ca (tip: download the RACEapp+ to your device from the Apple or Android stores). For more information, please visit South Island Division of Family Practice: RACE
- Vancouver Coastal Health Region/Providence Health Care: www.raceconnect.ca www.raceapp.ca (tip: download the RACEapp+ to your device from the Apple or Android stores)
- Compass: 1-855-702-7272 available Monday to Friday, 9am to 5pm
- Phone and telehealth consultations for practitioners working with children and youth living with mental health and substance use concerns. The Compass multidisciplinary team can help with diagnostic clarification, medication recommendations, treatment planning, consultation around Cognitive Behavioural Therapy, Dialectical Behavioural Therapy, substance use counselling, behavioural challenges, family challenges, trauma treatment, and general support when things aren't going well. You will receive a written record of all consultation recommendations for the patient's chart.
References
- Caring for Patients Who Have Experienced Trauma: ACOG Committee Opinion, Number 825. Obstet Gynecol. 2021 Apr;137(4):e94–9.
- Turpel-Lafond ME. In Plain Sight: Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care [Internet]. Ministry of Health; 2020. Available from: https://engage.gov.bc.ca/app/uploads/sites/613/2021/02/In-Plain-Sight-Data-Report_Dec2020.pdf1_.pdf
- Office of the Provincial Health Officer. Responding to British Columbia’s Drug Poisoning Crisis [Internet]. Ministry of Health; 2021. Available from: https://www2.gov.bc.ca/assets/gov/health/about-bc-s-health-care-system/office-of-the-provincial-health-officer/overdose-response-progress-update-jan-july-2021.pdf
- King TE, Wheeler MB. Medical Management of Vulnerable and Underserved Patients: Principles, Practice, and Populations [Internet [Internet]. 2nd ed. McGraw-Hill Medical; 2016. Available from: https://accessmedicine.mhmedical.com/book.aspx?bookid=1768
- Wilkinson T. Taking care of each other during COVID-19 – peer support for physicians [Internet]. UBC Faculty of Medicine; 2020 [cited 2023 Oct 18]. Available from: https://thischangedmypractice.com/peer-support-for-physicians-during-covid-19/
- Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From Treatment to Healing: The Promise of Trauma-Informed Primary Care. Womens Health Issues. 2015 May;25(3):193–7.
- Woodgate RL, Zurba M, Tennent P, Cochrane C, Payne M, Mignone J. A qualitative study on the intersectional social determinants for indigenous people who become infected with HIV in their youth. Int J Equity Health. 2017 Dec;16(1):132.
- Allan B, Smylie J. First Peoples, second class treatment: The role of racism in the health and well-being of Indigenous peoples in Canada [Internet]. The Wellesley Institute; 2015 [cited 2023 Aug 30]. Available from: https://www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf
- Howard HA. Canadian Residential Schools and Urban Indigenous Knowledge Production about Diabetes. Med Anthropol. 2014;33(6):529–45.
- Ellis WR, Dietz WH. A New Framework for Addressing Adverse Childhood and Community Experiences: The Building Community Resilience Model. Acad Pediatr. 2017 Sep;17(7):S86–93.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. REPRINT OF: Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 2019 Jun;56(6):774–86.
- Quinn J. 3 Realms of ACEs [Internet]. PACEs Connection; 2020. Available from: https://www.pacesconnection.com/blog/3-realms-of-aces-updated
- Group OPG. The Art of Difficult Conversations [Internet. Or Pain Guid Group [Internet]. 2022 Jan 26; Available from: https://www.oregonpainguidance.org/guideline/the-art-of-difficult-conversations/
- Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. J Pers Soc Psychol. 2010 Dec;99(6):1025–41.
- Torchalla I, Linden IA, Strehlau V, Neilson E, Krausz M. “Like a lots happened with my whole childhood”: Violence, trauma, and addiction in pregnant and postpartum women from Vancouver’s Downtown Eastside. Harm Reduct J. 2014;11(1):34.
- Center for Resilient Children, Mackrain M. Devereaux Adult Resilience Survey (DARS) [Internet]. Center for Resilient Children; 2013. Available from: https://centerforresilientchildren.org/wp-content/uploads/Devereux-Adult-Resilience-Survey-DARS_full.pdf
- Kornhaber R, Walsh K, Duff J, Walker K. Enhancing adult therapeutic interpersonal relationships in the acute health care setting: an integrative review. J Multidiscip Healthc. 2016 Oct;Volume 9:537–46.
- Kolk BA, Ducey CP. The psychological processing of traumatic experience: Rorschach patterns in PTSD. J Trauma Stress. 1989 Jul;2(3):259–74.
- SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach [Internet]. Substance Abuse and Mental Health Services Administration; 2014 [cited 2019 Sep 6]. Available from: https://store.samhsa.gov/system/files/sma14-4884.pdf
- Franco F. Understanding Intergenerational Trauma: An Introduction for Clinicians [Internet]. GoodTherapy. 2021. Available from: https://www.goodtherapy.org/blog/Understanding_Intergenerational_Trauma
- PHSA Ethics Service. PHSA Ethical Practice Guide [Internet]. Provincial Health Services Authority (PHSA); 2022. Available from: http://www.phsa.ca/our-services-site/Documents/PHSA%20Ethical%20Practice%20Guide%20Apr%202022.pdf
- Office of the Chief Medical Officer. Cultural Safety and Humility [Internet]. First Nations Health Authority (FNHA); Available from: https://www.fnha.ca/what-we-do/cultural-safety-and-humility
- Cicchetti D. Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry. 2010 Oct;9(3):145–54.
- Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010 Jul;30(5):479–95.
- Luthar SS, Cicchetti D, Becker B. The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child Dev. 2000 May;71(3):543–62.
- McEwen BS. In pursuit of resilience: stress, epigenetics, and brain plasticity. Ann N Y Acad Sci. 2016 Jun;1373(1):56–64.
- McDonald S. Staying strong during tough times with the “medicine of resilience” [Internet]. First Nations Health Authority (FNHA) News; 2020. Available from: https://www.fnha.ca/about/news-and-events/news/staying-strong-during-tough-times-with-the-medicine-of-resilience
- Warren J. Neuroplasticity: Building the Brain You Want [Internet]. Jared Warren; Available from: https://www.mybestself101.org/neuroplasticity
- Centers for Disease Control and Prevention (CDC). Fast Fact: Preventing Bullying [Internet]. Centers for Disease Control and Prevention (CDC); Available from: https://www.cdc.gov/violenceprevention/youthviolence/bullyingresearch/fastfact.html
- Adams E, Clarmont W. Intergenerational Trauma and Indigenous Healing. Visions Journal. 2016;11(4):7.
- Boivin, Michel, Hertzman, Clyde. Early Childhood Development: adverse experiences and developmental health. [Internet]. Ottawa: Royal Society of Canada - Canadian Academy of Health Sciences Expert Panel (with Ronald Barr, Thomas Boyce, Alison Fleming, Harriet MacMillan, Candice Odgers, Marla Sokolowski, & Nico Trocmé).; 2012 [cited 2019 Sep 6]. Available from: https://rsc-src.ca/sites/default/files/pdf/ECD%20Report_0.pdf
- King, Talmadge E., Wheeler, Margaret B. Medical Management of Vulnerable and Underserved Patients: Principles, Practice, and Populations [Internet]. 2nd ed. McGraw-Hill Medical; 2016 [cited 2019 Sep 6]. Available from: https://accessmedicine.mhmedical.com/book.aspx?bookid=1768
- Dolezal L, Gibson M. Beyond a trauma-informed approach and towards shame-sensitive practice. Humanit Soc Sci Commun. 2022 Jun 24;9(1):214.
|
BC Guidelines are developed for the Medical Services Commission by the Guidelines and Protocols Advisory Committee, a joint committee of Government and the Doctors of BC. BC Guidelines are adopted under the Medicare Protection Act and, where relevant, the Laboratory Services Act. Disclaimer: This extended learning document is based on best available scientific evidence and clinical expertise as of January 17, 2024. It is not intended as a substitute for the clinical or professional judgment of a health care practitioner. |


 TOP
TOP