6 - Cognitive impairment Including dementia - CCMTA Medical Standards
Cognitive impairment and dementia and medical fitness to drive.
6.1 About cognitive impairment and dementia
Cognitive impairment, also called cognitive dysfunction or neuropsychological impairment, refers to any impairment of a cognitive function such as:
- Memory
- Attention
- Language
- Problem solving, or
- Judgment
Cognitive impairment may have any number of causes including:
- Brain trauma
- Anoxia (lack of oxygen to the brain)
- Infection
- Toxicities, or
- Degenerative, metabolic or nutritional diseases
The presentation of cognitive impairment is variable depending on the cognitive functions affected and the degree of impairment. Cognitive impairment may progress to dementia, it may remain stable, or there may be a recovery of normal cognitive function.
Dementia
Dementia refers to a disorder characterized by memory impairment in conjunction with one or more other cognitive deficits. In North America, the most commonly used criteria for the diagnosis of a dementia are those articulated by the American Psychiatric Association.
DSM-5 retained the term "dementia" from the previous edition for continuity but replaced it officially with “major neurocognitive disorder”. It points out that dementia is generally associated with the older individual while a neurocognitive disorder was the term used for younger individuals with the same symptoms. Therefore DSM-5 advocates using the same term for individuals of all ages who manifest major cognitive limitations. However, since dementia is still an accepted term according to DSM-5 and is the term most commonly used by researchers and licensing authorities in referring to this condition, for simplicity it will continue to be used in this chapter. Neurocognitive disorders will be used when referring to all types of cognitive limitations.
The defining features of dementia are:
A. Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
1. Concern of the individual, a knowledgeable informant, or the clinician that there has been a significant decline in cognitive function; and
2. A substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment.
B. Cognitive deficits interfere with independence in everyday activities (i.e. at a minimum, requiring assistance with complex instrumental activities of daily living such as paying bills or managing medications).
C. The cognitive deficits do not occur exclusively during the context of a delirium.
D. The cognitive deficits are not better accounted for by another mental disorder (e.g. major depressive disorder, Schizophrenia)*.
(*DSM-5, p 591-645)
Dementia has many causes and more than 100 types of dementia have been documented. The five most common types of dementia are:
- Alzheimer’s disease
- Vascular dementia (multi-infarct dementia)
- Mixed Alzheimer’s and vascular dementia
- Dementia with Lewy bodies (Lewy body dementia), and
- Frontotemporal dementia (Pick’s disease or Pick’s complex). Frontotemporal dementia may not meet all of the criteria noted for dementia, especially in the early stages, but may still result in significant functional impairment.
These types of dementia are all progressive and irreversible, and are characterized by impairments in multiple cognitive functions.
In Alzheimer’s disease, the most common form of dementia, the earliest cognitive symptoms include difficulties in:
- Recent memory
- Word finding
- Confrontation naming
- Orientation, and
- Concentration
Characteristics of later stages include:
- Slowed rates of information processing
- Attentional deficits
- Disturbances in executive functions, and
- Impairments in language, perception and praxis
Less commonly, dementias can result from:
- Head injury and trauma
- Brain tumours
- Depression
- Hydrocephalus (excessive accumulation of cerebrospinal fluid (CFS) in the brain)
- Bacterial and viral infections
- Toxic, endocrine and metabolic causes, or
- Anoxia
Some of these dementias may be reversible. Specific examples of reversible causes of dementia include:
- Thyroid deficiency or excess
- Vitamin B12 deficiency
- Chronic alcoholism
- Abnormal calcium levels
- Dementia associated with celiac disease, and
- Intracranial space-occupying lesions
Treatment for dementia has become available over the last decade with cognition enhancing drugs such as donepezil (AriceptTM), galantamine (ReminylTM) and rivastigmine (ExelonTM). These drugs seem to improve symptoms of the disease in some stages of dementia but their therapeutic effect is variable. It is generally considered not likely that treatment with medication would improve cognition to a degree that would enable driving in those whose driving skills had declined to an unsafe level or those who had previously failed a driving assessment due to cognitive impairment.
Mild cognitive impairment
Mild cognitive impairment (MCI) is a term that usually refers to the transitional state between the cognitive changes associated with normal aging and the fully developed clinical features of dementia. The diagnostic criteria for MCI are evolving but in general it describes a cognitive decline that presents no significant functional impairment.
A simple summary of factors in determining degree of Dementia and Mild Cognitive Impairment include:
|
Mild cognitive Impairment (MCI) (Some memory impairment but dementia not definitively diagnosed) |
Mild Dementia (Mild neurocognitive disorder) |
Moderate Dementia (Major neurocognitive disorder) |
Severe Dementia (Major neurocognitive disorder) |
|
Forgets name, location of objects May have trouble finding words May have difficulty traveling to new locations May have difficulty with problems at work |
Has difficulty with complex tasks or instrumental activities of daily living (eg finances, shopping, planning dinner, cooking, taking medication, telephoning etc.) |
Has difficulty with basics activities of daily living (eg eating, dressing hygiene) Needs help choosing and putting on clothing Requires prompting and assistance when bathing |
Decreased ability to use toilet and is incontinent Vocabulary limited Loses ability to walk and sit Unable to smile |
Delirium
Delirium is a condition characterized by a disturbance of consciousness and a change in cognition that occurs over a relatively short period of time, usually hours to days.
Common causes of delirium include:
- Vascular disorders (e.g. stroke, myocardial infarct)
- Infections (e.g. urinary tract, chest)
- Drugs (e.g. analgesics, sedatives, alcohol, illicit drugs), and
- Metabolic disorders (e.g. renal failure, hepatic failure, endocrine disorders)
Although the symptoms of delirium may be similar to dementia, delirium is temporary and therefore considered a transient impairment for licensing purposes.
6.2 Prevalence
Estimates from the Canadian Study on Health and Aging (1991) suggest that 8% of all Canadians aged 65 and older meet the criteria for dementia, increasing to 34.5% for those 85 and older. A 2004 study projected that, in 2007, there would be 65,780 individuals with dementia in British Columbia, 44,130 of whom would have Alzheimer’s disease.
In relation to cognitive impairment from any cause that has not been diagnosed as dementia, research indicates that the prevalence is from 2% to 10% at age 65, and 2% to 25% by age 85*.
(* DSM-5, p. 608)
The prevalence of both cognitive impairment (all causes – not dementia) and dementia increases with age. As shown in the table below, when combined, the prevalence of mild and major neurocognitive disorders is 3% to 12% at age 65 and 35% to 55% by age 85*.
(* DSM-5, p. 608)
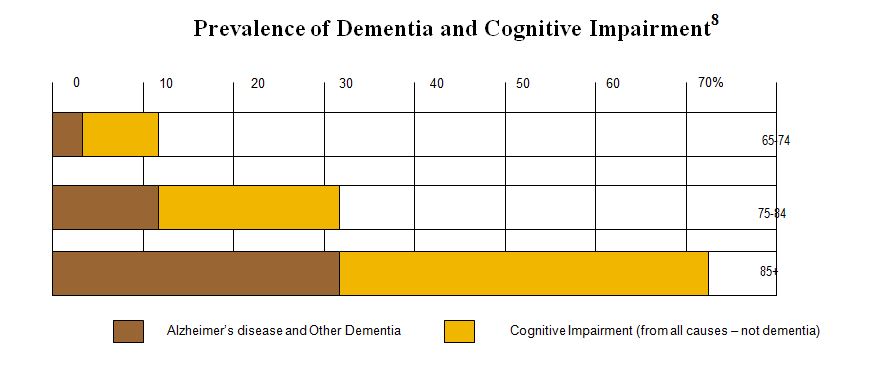
8 Source: Canadian Study of Health and Aging, 1991
6.3 Cognitive impairment, dementia and adverse driving outcomes
Research clearly indicates that, as a group, those with dementia are at higher risk for adverse driving outcomes. In particular, individuals with dementia who experience behavioural disturbances and who are treated with psychotropic medications (e.g. antipsychotics, antidepressants) may be at increased risk. It is important to note that studies also indicate that many individuals with dementia show no evidence of deterioration of driving skills in the early stages of their illness.
The significance of cognitive impairment and dementia in relation to driving was the subject of a study of a panel of experts in the context of the revision of the CMA medical guide.* Following an extensive review of the scientific literature, the study’s principal conclusions are:
1. Cognitive problems often have a direct effect upon fitness to drive and any indications of possible cognitive compromises of fitness to drive must not be neglected by clinicians.
2. Diagnosis of dementia alone is not sufficient to withdraw driving privileges.
3. Severe dementia is an absolute contraindication to driving.
4. No in-office test or battery of tests, including global cognitive screens such as MMSE or MoCA have sufficient sensitivity or specificity to be used as the sole determinant of driving fitness in all cases. However, abnormalities in these tests indicate a requirement for further testing.
5. Patients with dementia who are deemed fit to drive should be re-evaluated every 6 to 12 months or sooner, if indicated.
6. A clinician with doubts about a patient’s cognitive functioning and its effects upon driving should refer the patient for a functional driving assessment by an occupational therapist or directly to the licensing authority.
7. As with many disabling progressive diseases that lead to driving cessation, conversations regarding eventual retirement from driving should be held as early as possible.
(*Report, 2016)
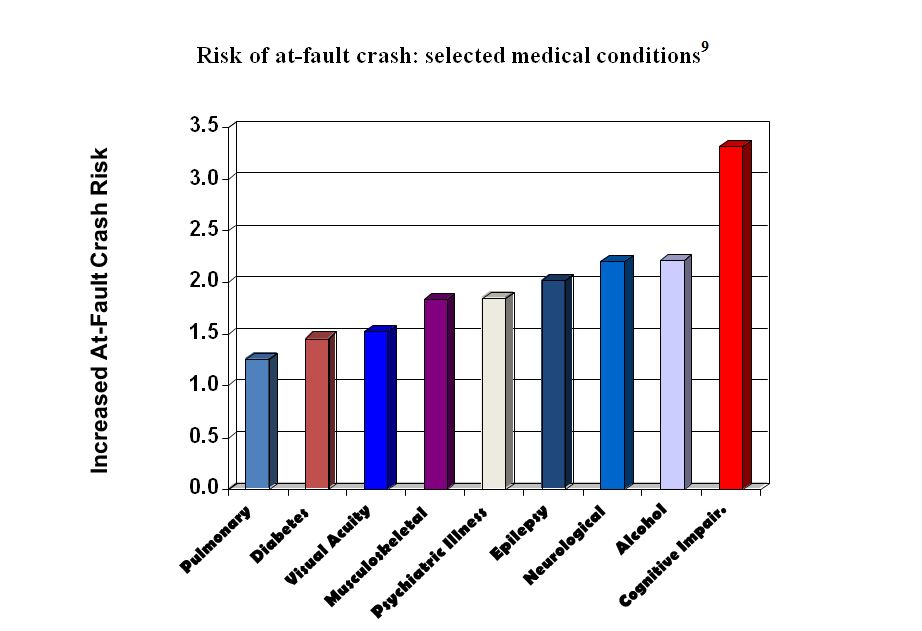
(9 Source: Diller, E, Cook, L, Leonard, D, Reading, J, Dean, JM, Vernon, D. Evaluating drivers licensed with medical conditions in Utah, 1992-1996. DOT HS 809 023. Washington, DC: National Highway Traffic Safety Administration.)
6.4 Effect on functional ability to drive
| Condition | Type of driving impairment and assessment approach | Primary functional ability affected | Assessment tools |
|
Cognitive impairment Dementia |
Persistent impairment: Functional assessment | Cognitive |
Medical assessments Functional Assessment |
Cognitive impairments of any nature may, or may not, affect driver fitness since there is no uniform range of effects. There is no standard set of limitations, and they can vary greatly from one person to the other.
In the case of MCI the effects may be subtle and difficult to assess in an office setting.
Judgement and insight are important for driving yet the usual battery of tests used to assess the extent of cognitive limitations do not evaluate these functions. Hence, a functional driving assessment is usually the most appropriate means of assessing the effects of the cognitive limitations upon driving unless severe dementia has been demonstrated.
(Source:Diller, E, Cook, L, Leonard, D, Reading, J, Dean, JM, Vernon, D. Evaluating drivers licensed with medical conditions in Utah, 1992-1996. DOT HS 809 023. Washington, DC: National Highway Traffic Safety Administration)
6.5 Compensation
Drivers with cognitive impairment or dementia are not able to compensate for their functional impairment.
Requiring the cognitively-impaired driver to be accompanied by another person (co-pilot) or the imposition of geographical or any other restrictions (conditional licences) are not permitted.
6.6 Guidelines for Assessment
6.6.1 Cognitive impairment or dementia
| National Standard |
Eligible for any class licence if
|
| BC Guidelines |
|
| Conditions for maintaining licence | No conditions required |
| Reassessment |
|
| Information from health care providers |
|
| Rationale |
|
6.6.2 Severe dementia
| National Standard | Ineligible for any class of licence |
| BC Guidelines |
|
| Conditions for maintaining licence | Details of diagnosis |
| Reassessment | N/A |
| Information from health care providers | N/A |
| Rationale | A diagnosis of severe dementia indicates cognitive function is impaired to a degree that is unsafe for driving |
