7 - Diabetes and hypoglycemia - CCMTA Medical Standards
Diabetes, hypoglycemia and medical fitness to drive.
- 7.6.1 Type 2 diabetes – All drivers
- 7.6.2 Type 1 or type 2 diabetes treated with insulin – Non-commercial drivers
- 7.6.3 Type 1 or type 2 diabetes treated with insulin – Commercial drivers
- 7.6.4 Episode of severe hypoglycemia – Non-commercial drivers - Also applies to severe hypoglycemia while sleeping
- 7.6.5 Episode of hypoglycemia unawareness within past year – Non-commercial drivers
- 7.6.6 Persistent hypoglycemia unawareness – Non-commercial drivers
- 7.6.7 Episode of severe hypoglycemia – Commercial drivers - Also applies to severe hypoglycemia while sleeping
- 7.6.8 Episode of hypoglycemia unawareness in the last year– Commercial drivers
- 7.6.9 Persistent hypoglycemia unawareness – Commercial drivers
- 7.6.10 Summary Table of Diabetes Conditions and Driver Medical Standards
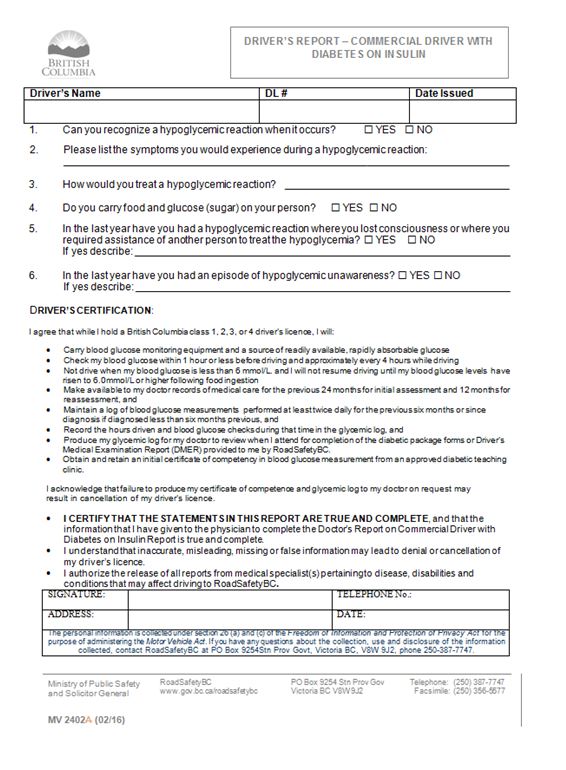
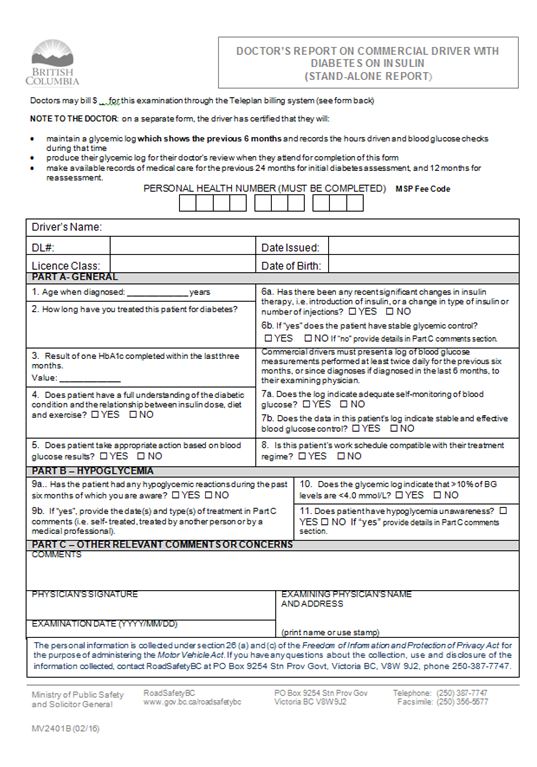
- 7.6.11 Doctor’s report on commercial driver with diabetes on insulin
- 7.6.12 Driver’s report – commercial driver with diabetes on insulin
7.1 About diabetes and hypoglycemia
Diabetes
Diabetes is a chronic and progressive disease characterized by hyperglycemia (high blood glucose). It appears in two principal forms*:
- Type 1 diabetes, formerly called insulin-dependent diabetes mellitus (IDDM) or juvenile diabetes, and
- Type 2 diabetes, formerly called non-insulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes
Type 1 and type 2 also differ in the underlying defect, and type of therapeutic control.
(*Other types of diabetes include gestational diabetes, other specific types (those due to genetic defects in β-cell function, genetic defects in insulin action, diseases of the exocrine pancreas, drug or chemical induced diabetes, etc.), and pre-diabetes. These types of diabetes are less common than type 1 and type 2 diabetes and are not discussed in this chapter.)
Type 1 diabetes
Type 1 diabetes can occur at any age, but it primarily appears before age 30. It is characterized by the inability to produce insulin and often more marked fluctuations in blood glucose. Daily insulin injections are always required to manage type 1 diabetes.
Type 2 diabetes
Type 2 diabetes usually occurs in individuals over the age of 40. It is characterized by an impaired ability to recognize and utilize insulin, and eventually diminished insulin production. Therapeutic control often is achieved by diet alone, or in combination with oral antihyperglycemic agents**, but people with type 2 diabetes whose blood glucose cannot be controlled in this way require treatment with insulin.
(**Oral antihyperglycemics also may be referred to as oral hypoglycemics)
Hypoglycemia
Anyone who requires treatment with insulin is at risk of hypoglycemia. Those with type 2 diabetes treated with insulin secretagogues (oral medications that stimulate the secretion of insulin) or metformin (an oral medication that enhances the effect of insulin) also may experience hypoglycemia, although the frequency with this treatment is lower than with insulin
Hypoglycemia may occur for a number of reasons, including reduced food intake, unusual level of physical exertion, and alteration of insulin dose.
Hypoglycemia can result in two types of symptoms, neurogenic (autonomic) and neuroglycopenic.
Neurogenic symptoms of hypoglycemia
The body’s immediate response to low blood sugar is to secrete hormones that counteract insulin, including adrenaline. The presence of adrenaline causes neurogenic (or autonomic) symptoms such as tremulousness, palpitations, anxiety, sweating, hunger and paresthesias (tingling and numbness). People with diabetes learn to recognize these symptoms as evidence of hypoglycemia and respond by consuming sugary liquids or starchy foods to increase their blood glucose level.
Neuroglycopenic symptoms of hypoglycemia
Neuroglycopenic symptoms are the direct result of impaired brain function due to low glucose levels. These symptoms include confusion, weakness or fatigue, severe cognitive failure, seizure and coma. As the blood glucose level falls, higher cortical function (insight, judgment, calculation, speech and memory) is the first to be affected. Next, a person will experience stupor, characterized by confusion, slurred speech, slow reaction times, poor judgment and lack of coordination. If the level continues to fall, there will be loss of consciousness, seizures and potentially brain damage or death.
Hypoglycemia unawareness
Another complicating factor is hypoglycemia unawareness, which is the inability to recognize the autonomic symptoms of hypoglycemia or a failure of such warning signs to occur prior to impaired brain function. If the initial autonomic symptoms caused by the release of adrenaline are missed, a person experiencing hypoglycemia can only rely on the neuroglycopenic symptoms as an indicator of low blood glucose. Because these symptoms appear in the context of cognitive impairment, they are not easily recognized by the hypoglycemic individual and may delay or prevent self-treatment.
Severe hypoglycemia
Severe hypoglycemia is commonly defined as hypoglycemia that requires outside intervention to abort, or that produces an alteration in level of consciousness or loss of consciousness. The altered or reduced level of consciousness prevents a person experiencing severe hypoglycemia from taking appropriate action.
7.2 Prevalence
Diabetes
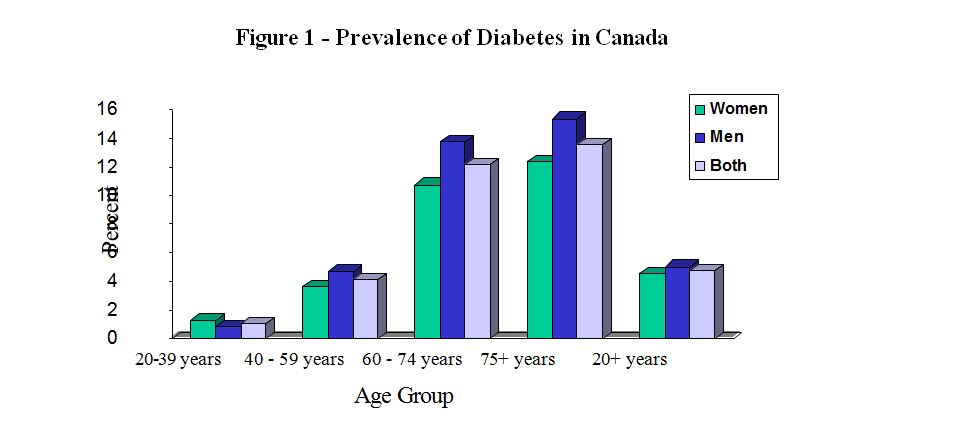
Based on research conducted by the National Diabetes Surveillance System, it is estimated that approximately 5% of Canadians aged 20 years and older have been diagnosed with diabetes. Diabetes is somewhat more prevalent in males, and the
overall prevalence of diabetes increases with age, as shown in the figure below. It is estimated that 5 to 10% of diagnosed diabetes is type 1, and 90 to 95% is type 2.
Hypoglycemia
A study of people with type 1 diabetes conducted in 1993 estimated that the incidence of mild hypoglycemia (hypoglycemia for which a person is able to treat themselves) to be 28 episodes per person per year. The incidence of severe hypoglycemia was estimated to be 0.31 episodes per person, per year. Since the mid 1990’s there has been an increased therapeutic emphasis on tight glycemic control, which has been shown to significantly reduce the complications of diabetes. Unfortunately, the use of more intensive treatment to maintain glycemic control has increased the risk of hypoglycemia by as much as two or three times. This suggests that these estimates on the prevalence of hypoglycemia in type 1 diabetes may be low.
While people with type 2 diabetes who are treated with insulin are at risk of hypoglycemia, the frequency is lower than for those with type 1 diabetes. The incidence of severe hypoglycemia for type 2 diabetes treated with insulin secretagogues is about 1 to 2% per year, with higher risk for longer use, older age, and the use of chlorpropamide and other long-acting secretagogues. The concomitant use of beta blockers and insulin previously has been thought to increase the risk of hypoglycemia; however, this theoretical concern is not often seen in practice.
For anyone with diabetes, a history of severe hypoglycemia, hypoglycemia unawareness, and low blood glucose levels are consistent predictors of future hypoglycemia.
Hypoglycemia unawareness
It is estimated that 25% of all those treated with insulin will experience one or more episodes of hypoglycemia unawareness. In type 1 diabetes, hypoglycemia unawareness increases with the duration of diabetes and the likelihood increases if autonomic neuropathy is present. In type 2 diabetes, hypoglycemia unawareness is relatively uncommon.
Factors that may be associated with hypoglycemia unawareness include older age, duration of diabetes, presence of autonomic neuropathy, species of insulin, degree of metabolic control, and number of hypoglycemic events.
7.3 Diabetes and adverse driving outcomes
Over the last twenty years the scientific evidence on the relationship between diabetes and crash risk has evolved, in part as a reflection of better management and control. Although there is some variability in results of research on drivers with diabetes, there is clear evidence to show that both non-commercial and commercial drivers with diabetes are at an increased risk of motor vehicle crashes.
It has been shown that diabetes treatment modality is an important consideration in determination of risk for drivers. Study results consistently indicate that individuals taking insulin have an elevated risk of crashes. Some studies have also shown an elevated risk of crash for drivers with type 2 diabetes who are treated with a combination of oral antihyperglycemics (secretagogues and non-secretagogues). Those treated by diet alone or with a single oral antihyperglycemic agent have shown no elevated risk of crash.
A relationship between hypoglycemia and crashes has also been found. Despite a lack of data from studies of large samples of people with diabetes, a number of small studies have shown a relationship between hypoglycemic reactions and motor vehicle crashes.
While research has established clear links between diabetes, hypoglycemia and motor vehicle crashes, the variable results of these studies indicate that decisions about driving should be based on assessment of individual medical history and circumstances including:
- Treatment modality
- Incidence of hypoglycemia
- Incidence of hypoglycemia unawareness, and
- Presence of chronic complications of diabetes
7.4 Effect on functional ability to drive
| Condition | Type of driving impairment and assessment approach | Primary functional ability affected | Assessment tools |
| Severe hypoglycemia | Episodic impairment: Medical assessment – likelihood of impairment | All – sudden incapacitation | Medical assessments |
For individuals with diabetes, both acute and chronic complications of the disease may affect fitness to drive.
Hyperglycemia may cause blurred vision, confusion, and eventually diabetic coma. For the purposes of this standard, these are considered transient impairments.
The neuroglycopenic symptoms associated with severe hypoglycemia can significantly impair the sensory, motor and cognitive functions required for driving. There are studies that suggest that mild hypoglycemia may also impair these functions.
While it is clear that the risk of hypoglycemia is an important consideration when assessing the fitness of drivers with diabetes, research indicates that the chronic complications of diabetes are more likely to be responsible for impaired fitness to drive than episodic incidents of hypoglycemia. Over time, people with diabetes often develop co-morbidities caused by their prolonged exposure to hyperglycemia. These complications of diabetes include retinopathy, neuropathy, nephropathy, cardiovascular disease and peripheral vascular disease. Therefore, the effect of chronic complications always must be considered when assessing fitness to drive for people with diabetes.
7.5 Compensation
As severe hypoglycemia is an episodic impairment, a driver cannot compensate.
7.6 Guidelines for Assessment
7.6.1 Type 2 diabetes - All drivers
- Treated with diet and exercise alone or
- Oral medication - non insulin secretagogues medication, i.e. metformin, or
- Oral medication - insulin secretagogues i.e. glyburide, diamicron, etc
| National Standard |
All drivers eligible for any licence class if:
|
| BC Guidelines |
|
| Conditions for maintaining licence |
|
| Reassessment |
If on Oral Medications and Non-Insulin Secretagogues
If on Oral Insulin-Secretagogues
|
| Information from health care providers | Description of treatment |
| Rationale |
|
7.6.2 Type 1 or type 2 diabetes treated with insulin - Non-commercial drivers
| National Standard |
Non-commercial drivers eligible for a licence if:
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request:
|
| Conditions for maintaining licence |
|
| Reassessment | If blood glucose levels and treatment are not stable, RoadSafetyBC will re-assess annually until levels and treatment are stable. If blood glucose levels and treatment are stable, RoadSafetyBC will re-assess every five years, or in accordance with the schedule for age-related re-assessment |
| Information from health care providers |
|
| Rationale | Drivers with diabetes who are treated with insulin therapy are at risk for hypoglycemia. In addition to the conditions regarding how to avoid severe hypoglycemia while driving that apply to drivers treated with insulin secretagogues, there are additional conditions for checking and monitoring blood glucose. These conditions are based on guidelines published by Diabetes Canada. |
7.6.3 Type 1 or type 2 diabetes treated with insulin - Commercial drivers
| Standard |
Commercial driver eligible for a licence if:
|
| BC Guidelines |
|
| Conditions for maintaining licence |
|
| Reassessment | RoadSafetyBC will re-assess annually |
| Information from health care providers |
|
| Rationale |
|
| Restrictions | No restrictions required |
7.6.4 Episode of severe hypoglycemia - Non-commercial drivers - Applies also to severe hypoglycemia while sleeping
| Standard |
Non-commercial drivers eligible for a licence if:
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request:
|
| Conditions for maintaining licence |
|
| Reassessment |
RoadSafetyBC will re-assess as recommended by the treating physician. At that time, if the treating physician indicates that there have been no episodes of severe hypoglycemia within the past six months, the application guidelines for private drivers with diabetes will apply |
| Information from health care providers |
|
| Rationale | Severe hypoglycemia indicates a lack of glycemic control and the potential for further hypoglycemic episodes. Once control is re- established and driving resumes, more stringent glucose monitoring conditions are required temporarily to mitigate the increased risk of hypoglycemia |
7.6.5 Episode of hypoglycemia unawareness within past year - Non-commercial drivers
| National Standard |
Non-commercial drivers eligible for a licence if:
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request:
|
| Conditions for maintaining licence |
|
| Reassessment | RoadSafetyBC will re-assess in one year. At that time, if the treating physician indicates that there have been no further episodes of hypoglycemia unawareness within the past year, the conditions listed above will be removed and the applicable guidelines for private drivers with diabetes will apply |
| Information from health care providers |
|
| Rationale | Hypoglycemia unawareness greatly increases the risk for hypoglycemia while driving. This standard requires that glycemic awareness be re-established before driving resumes. Once awareness and glucose stability are re-established, more stringent glucose monitoring guidelines are required temporarily to mitigate the increased risk of hypoglycemia |
7.6.6 Persistent hypoglycemia unawareness - Non-commercial drivers
| National Standard |
Non-commercial drivers eligible for a licence if:
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request
|
| Conditions for maintaining licence |
|
| Reassessment |
|
| Information from health care providers |
|
| Rationale | Persistent hypoglycemia unawareness presents the greatest risk for hypoglycemia while driving. The standard permits non-commercial drivers to continue to drive provided they are able to maintain stable blood glucose levels and follow more stringent glucose monitoring requirements |
7.6.7 Episode of severe hypoglycemia - Commercial drivers - Applies also to severe hypoglycemia while sleeping
| Standard |
Commercial drivers eligible for a licence if:
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request:
|
| Conditions for maintaining licence |
|
| Reassessment | RoadSafetyBC will re-assess annually |
| Information from health care providers |
|
| Rationale | Severe hypoglycemia indicates a lack of glycemic control and the potential for further hypoglycemic episodes. Once control is re- established and driving resumes, more stringent glucose monitoring conditions are required temporarily to mitigate the increased risk of hypoglycemia |
7.6.8 Episode of hypoglycemia unawareness in the last year - Commercial drivers
| National Standard |
Commercial drivers eligible for a licence if
|
| BC Guidelines |
If further information is required, RoadSafetyBC may request
|
| Conditions for maintaining licence |
|
| Reassessment | RoadSafetyBC will re-assess in one year. At that time, if the treating physician indicates that there have been no episodes of hypoglycemia unawareness within the past year, the conditions listed above will be removed and the applicable guidelines for commercial drivers with diabetes will apply |
| Information from health care providers |
|
| Rationale | Hypoglycemia unawareness greatly increases the risk for hypoglycemia while driving. This standard requires that glycemic awareness be re-established before driving resumes. Once awareness and glucose stability are re-established, more stringent glucose monitoring guidelines are required temporarily to mitigate the increased risk of hypoglycemia |
7.6.9 Persistent hypoglycemia unawareness - Commercial drivers
| National Standard | Commercial drivers not eligible for a licence |
| BC Guidelines | RoadSafetyBC will not generally request further information |
| Conditions for maintaining licence | N/A |
| Reassessment | N/A |
| Information from health care providers | N/A |
| Rationale | Persistent hypoglycemia unawareness presents the greatest risk for hypoglycemia while driving. Given the increased driving exposure associated with commercial driving, individuals who have persistent hypoglycemia unawareness are not fit to drive |
7.6.10 Summary table of diabetes conditions and driver medical standards
| Type II | Standard |
|---|---|
| Non-Commercial | Eligible for licence |
| Commercial | Eligible for licence |
| Type I or Type II Insulin-Treated | Standard |
| Non-Commercial | Eligible for licence |
| Commercial |
Eligible for licence
|
| Severe Hypoglycemia Episode | Standard |
| Non-Commercial |
Eligible for licence
|
| Commercial |
Eligible for licence
|
| Episode of Hypoglycemic Unawareness | Standard |
| Non-Commercial |
Eligible for licence
|
| Commercial |
Eligible for licence
|
| Persistent Hypoglycemic Unawareness | Standard |
| Non-Commercial |
Eligible for licence
|
| Commercial | Ineligible to Drive |
7.6.11 Doctor's report on commercial driver with diabetes on insulin
7.6.12 Driver's report - Commercial drivers with diabetes on insulin